A registered nurse (RN) and an experienced licensed practical nurse (LPN) are caring for a group of clients. Which of the following tasks should the RN delegate to the LPN? SELECT ALL THAT APPLY
Initiate a plan of care for a client who is postoperative from an appendectomy.
Administer a tap-water enema to a client who is preoperative.
Provide discharge instructions to a confused client's spouse.
Catheterize a client who has not voided in 8 hours.
Obtain vital signs from a client who is 6 hours postoperative.
Correct Answer : B,D,E
Choice A reason: Initiating a plan of care for a client who is postoperative from an appendectomy is not a task that the RN should delegate to the LPN, as it requires nursing judgment, critical thinking, and assessment skills that are beyond the scope of practice of the LPN. The RN is responsible for developing, implementing, and evaluating the plan of care for each client based on their individual needs, preferences, and goals. The RN can delegate some aspects of the plan of care to the LPN, such as performing routine tasks or monitoring the client's status, but the RN must supervise and evaluate the LPN's performance.
Choice B reason: Administering a tap-water enema to a client who is preoperative is a task that the RN can delegate to the LPN, as it is a standardized procedure that does not require nursing judgment or assessment. The LPN has the knowledge and skills to perform this task safely and effectively, following the established policies and protocols of the facility. The RN should provide clear instructions and expectations to the LPN, such as the type, amount, and temperature of the solution, the position and comfort of the client, and the signs and symptoms to report. The RN should also verify that the LPN has completed the task and documented the outcome.
Choice C reason: Providing discharge instructions to a confused client's spouse is not a task that the RN should delegate to the LPN, as it involves teaching, counseling, and evaluating the client's and family's understanding and readiness for discharge. These are complex activities that require nursing judgment, communication skills, and evaluation skills that are beyond the scope of practice of the LPN. The RN is responsible for ensuring that the client and family receive adequate information and education about the client's condition, treatment, medications, follow-up care, and community resources. The RN can delegate some aspects of discharge planning to the LPN, such as collecting data or providing reinforcement of teaching, but the RN must supervise and evaluate the LPN's performance.
Choice D reason: Catheterizing a client who has not voided in 8 hours is a task that the RN can delegate to the LPN, as it is a standardized procedure that does not require nursing judgment or assessment. The LPN has the knowledge and skills to perform this task safely and effectively, following the established policies and protocols of the facility. The RN should provide clear instructions and expectations to the LPN, such as the type and size of the catheter, the sterile technique, and the urine output measurement. The RN should also verify that the LPN has completed the task and documented the outcome.
Choice E reason: Obtaining vital signs from a client who is 6 hours postoperative is a task that the RN can delegate to the LPN, as it is a routine task that does not require nursing judgment or assessment. The LPN has the knowledge and skills to perform this task safely and effectively, using appropriate equipment and techniques. The RN should provide clear instructions and expectations to the LPN, such as the frequency and parameters of vital signs monitoring. The RN should also verify that the LPN has completed the task and documented the outcome.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A: Encourage community members to practice fire drills. This is incorrect because fire drills are a part of the preparedness phase, not the prevention/mitigation phase. The prevention/mitigation phase aims to reduce the risk and impact of disasters, while the preparedness phase aims to enhance the readiness and response capacity of individuals and communities.
Choice B: Identify community members who have disabilities. This is incorrect because identifying community members who have disabilities is also a part of the preparedness phase, not the prevention/mitigation phase. The prevention/mitigation phase focuses on actions that can prevent or minimize the occurrence or effects of disasters, such as installing smoke detectors, reinforcing buildings, or creating evacuation routes.
Choice C: Provide first aid to community members affected by a tornado. This is incorrect because providing first aid to community members affected by a tornado is a part of the response phase, not the prevention/mitigation phase. The response phase involves immediate actions to save lives, protect property, and meet basic needs after a disaster occurs.
Choice D: Assist community members in developing a disaster plan. This is correct because assisting community members in developing a disaster plan is a part of the prevention/mitigation phase. A disaster plan can help identify potential hazards, assess vulnerabilities, establish goals and objectives, and implement strategies to reduce the risk and impact of disasters.
Correct Answer is A
Explanation
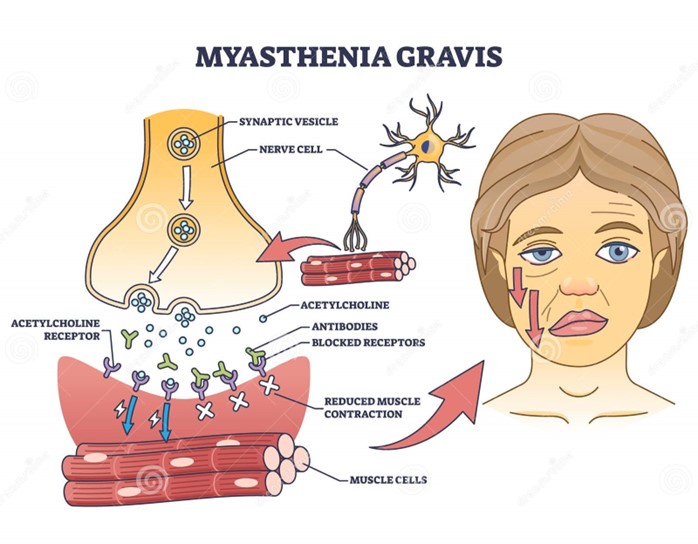
Choice A reason: Planning medication doses to occur before meals is a good suggestion to improve the client's nutritional status. Myasthenia gravis is a neuromuscular disorder that causes weakness and fatigue of the voluntary muscles, especially those involved in chewing and swallowing. Taking anticholinesterase medications before meals can enhance muscle strength and coordination, and make it easier for the client to eat and avoid choking or aspiration.
Choice B reason: Restricting drinking fluids before and during meals is not a good suggestion to improve the client's nutritional status. Fluid intake is important for hydration and digestion, and should not be limited unless there is a medical reason, such as fluid overload or heart failure. Drinking fluids before and during meals can also help lubricate the food and prevent dryness or irritation of the mouth and throat.
Choice C reason: Increasing the amount of fat and carbohydrates in meals is not a good suggestion to improve the client's nutritional status. Fat and carbohydrates are sources of energy, but they can also increase the risk of obesity, diabetes, or cardiovascular disease if consumed excessively. A balanced diet that includes adequate protein, vitamins, minerals, and fiber is more beneficial for the client's health and well-being.
Choice D reason: Eating three large meals per day is not a good suggestion to improve the client's nutritional status. Eating large meals can be difficult and exhausting for the client with myasthenia gravis, as their muscle strength and endurance may decline over time. Eating smaller and more frequent meals can help maintain the energy level and prevent fatigue or hunger.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
