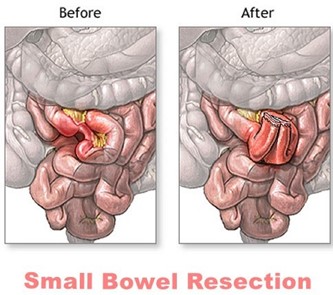
A patient reports gas pains and abdominal distention 2 days after a small bowel resection. Which nursing action should the nurse take?
Administer morphine sulfate.
Encourage the patient to ambulate.
Offer the prescribed promethazine.
Instill a mineral oil retention enema.
The Correct Answer is B
Gas pains and abdominal distention are common postoperative complications following small bowel resection. Ambulation is a simple and effective nursing intervention that can help alleviate these symptoms. Walking helps stimulate peristalsis, which can help move gas and stool through the gastrointestinal tract. It can also help prevent postoperative complications such as pneumonia and deep vein thrombosis.
Administering morphine sulfate (option A) may relieve pain, but it can also worsen constipation and abdominal distention. Promethazine (option C) is an antiemetic medication and may be helpful if the patient is experiencing nausea, but it is not the best intervention for gas pain and abdominal distention. Instilling a mineral oil retention enema (option D) may also be helpful in some cases, but it is not typically the first intervention for these symptoms and should be ordered by a healthcare provider.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["A","B","E"]
Explanation
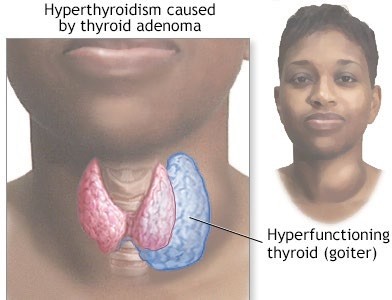
Answer c is incorrect because hyperthyroidism typically causes hypertension, not hypotension. Answer d is also incorrect because hyperthyroidism typically causes increased, not decreased, deep tendon reflexes. Answer f is incorrect because hyperthyroidism typically causes diarrhea, not constipation.
Correct Answer is A
Explanation
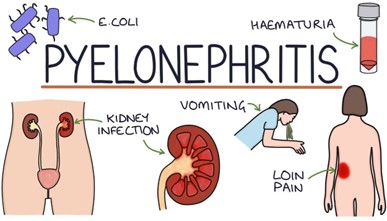
The most helpful finding by the nurse in determining whether a 67-yr-old patient with benign prostatic hyperplasia has an upper urinary tract infection (pyelonephritis) would be
**costovertebral tenderness**⁴. This is because costovertebral tenderness is a common symptom of pyelonephritis⁵. Pyelonephritis is an infection of the upper urinary tract that can cause fever, chills, flank pain, nausea, vomiting, and costovertebral tenderness⁵. Foul-smelling urine and bladder distention are not specific symptoms of pyelonephritis⁵. Suprapubic discomfort can be a symptom of lower urinary tract infection⁵.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
