A patient is admitted for treatment of Cushing's syndrome. The nurse correlates this disease process to which alteration in endocrine function?
Decreased cortisol level.
Elevated glucocorticoid level.
Decreased aldosterone secretion.
Elevated insulin secretion.
The Correct Answer is B
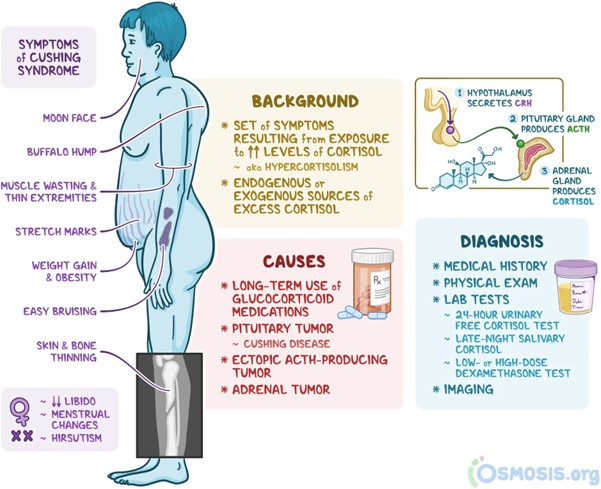
Cushing's syndrome is a disorder characterized by excessive production or prolonged exposure to high levels of glucocorticoids, particularly cortisol. This can occur due to various reasons, such as the use of corticosteroid medications or overproduction of cortisol by the adrenal glands. Elevated glucocorticoid levels result in a variety of clinical manifestations associated with Cushing's syndrome, including weight gain, central obesity, muscle wasting, thinning of the skin, easy bruising, and impaired glucose metabolism.
It's important to note that Cushing's syndrome can have different underlying causes, such as adrenal tumors, pituitary tumors, or ectopic ACTH production. Regardless of the cause, the common feature in Cushing's syndrome is the excessive glucocorticoid levels, which contribute to the signs and symptoms of the condition.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Prednisone is a corticosteroid medication that can increase blood glucose levels by promoting gluconeogenesis (the production of glucose from non-carbohydrate sources) and reducing glucose utilization in the body. This can lead to elevated blood sugar levels, especially in individuals with diabetes. The client's history of urinary tract infection and the use of Prednisone suggest that the infection might have triggered the development of DKA.
It's important to note that DKA can occur even when a person is taking insulin as prescribed and following their diet carefully if other factors contribute to the development of DKA, such as an underlying infection or the use of certain medications like Prednisone. The nurse should further assess the client's condition and notify the healthcare provider to initiate appropriate management for DKA.
Correct Answer is B
Explanation
A likely cause of a low sodium level (hyponatremia) of 128 mEq/L is the administration of hypotonic IV fluids. Hypotonic IV fluids have a lower concentration of solutes compared to the body's fluids, which can lead to dilutional hyponatremia. When these fluids are administered, they can cause water to move into the cells, diluting the sodium concentration in the bloodstream.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
