Related Questions
Correct Answer is D
Explanation
Choice A Reason: This is incorrect because mosquitoes do not transmit HIV. HIV is a virus that infects human cells and cannot survive in insects. Mosquitoes do not inject blood from one person to another when they bite, but only saliva that contains anticoagulants and enzymes.
Choice B Reason: This is incorrect because accidental puncture wounds are not a common mode of HIV transmission. HIV can be transmitted through exposure to infected blood or body fluids, such as through needle sharing, blood transfusion, or occupational injury. However, these cases are rare and can be prevented by using sterile equipment, screening blood products, and following universal precautions.
Choice C Reason: This is incorrect because casual contact is not a mode of HIV transmission. HIV is not an airborne virus and cannot be spread by coughing, sneezing, or breathing. HIV cannot be transmitted by hugging, kissing, or sharing utensils.
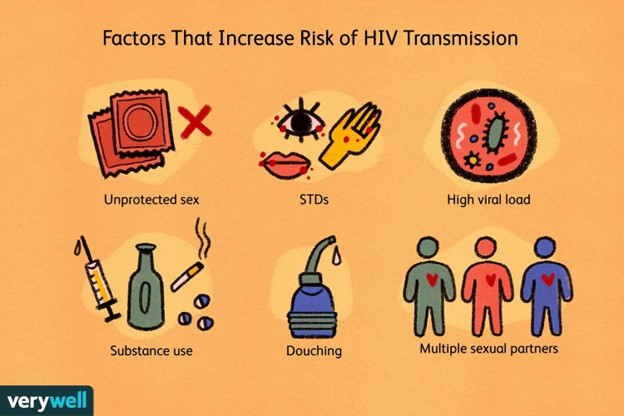
Choice D Reason: This is correct because direct contact with infected body fluids is the most common mode of HIV transmission. HIV can be transmitted through unprotected vaginal, anal, or oral sex with an infected person, as these activities can involve contact with infected blood, semen, vaginal fluid, or pre-ejaculate. HIV can also be transmitted through sharing needles or syringes with an infected person, or from mother to child during pregnancy, childbirth, or breastfeeding.
Correct Answer is C
Explanation
Choice A Reason: This is incorrect because sickle-cell anemia is a genetic disorder that affects the shape and function of red blood cells. It does not affect the AFP level, which is a protein produced by the fetus and placenta. Sickle-cell anemia can be detected by other prenatal tests, such as hemoglobin electrophoresis or DNA analysis.
Choice B Reason: This is incorrect because cardiac defects are structural abnormalities of the heart or blood vessels that affect the blood flow and oxygen delivery to the fetus. They may cause an increased AFP level, not a decreased one, as they can lead to fetal distress or edema. Cardiac defects can be detected by other prenatal tests, such as fetal echocardiography or ultrasound.
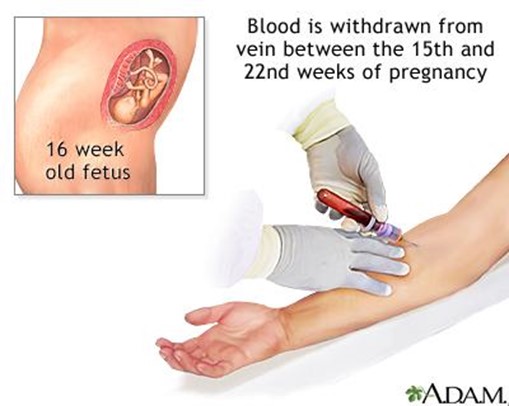
Choice C Reason: This is correct because Down syndrome is a chromosomal disorder that results from an extra copy of chromosome 21. It causes various physical and mental developmental delays and defects in the fetus. It is associated with a decreased AFP level, as well as decreased levels of human chorionic gonadotropin (hCG) and unconjugated estriol (uE3). Down syndrome can be confirmed by other prenatal tests, such as amniocentesis or chorionic villus sampling (CVS).
Choice D Reason: This is incorrect because respiratory disorders are problems that affect the breathing and gas exchange of the fetus. They may cause an increased AFP level, not a decreased one, as they can lead to fetal distress or edema. Respiratory disorders can be detected by other prenatal tests, such as fetal biophysical profile (BPP) or nonstress test (NST).