A nurse is working with two assistive personnel (AP). The nurse notes that one of the APs has been taking long breaks and making personal phone calls. Which of the following statements should the nurse make to resolve this conflict?
"Several staff members have commented that you don't do your fair share of the work."
"You have been very inconsiderate of others by not completing your share of the work."
"If you don't do your share of the work, I will have to inform the nurse manager."
"I need to talk to you about unit expectations regarding the timely completion of tasks."
The Correct Answer is D
The nurse should make the statement "I need to talk to you about unit expectations regarding timely completion of tasks" to resolve the conflict with the AP who has been taking long breaks and making personal phone calls. This statement is assertive and focuses on the issue at hand without blaming or attacking the AP. It also opens up a dialogue between the nurse and the AP to discuss the issue and find a resolution.
The other statements are not effective in resolving the conflict. Statements such as "Several staff members have commented that you don't do your fair share of the work" [a] and "You have been very inconsiderate of others by not completing your share of the work" [b] are accusatory and may make the AP defensive.
Threatening to inform the nurse manager [c] may also escalate the conflict and is not a constructive way to address the issue.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
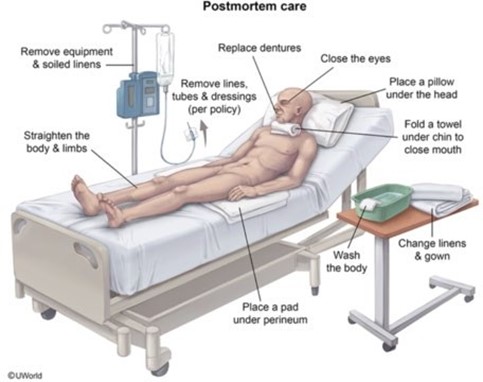
Assistive personnel (AP), also known as unlicensed assistive personnel (UAP), can perform tasks such as assisting with activities of daily living, hygiene, and nutrition, as well as those tasks that support professional nursing assessments ². Providing postmortem care for a client who has died [d] is a task that can be delegated to an AP.
The other options are not tasks that should be delegated to an AP. Educating a client on the use of a blood glucose monitor [a] involves patient education, which is typically the responsibility of a licensed nurse.
Interpreting a client's vital signs [b] involves assessing the client's health status, which is also typically the responsibility of a licensed nurse. Performing a central line dressing change for a client [c] is a complex task that requires specialized knowledge and skills.
Correct Answer is A
Explanation
The nurse should give the statement "I will notify the charge nurse of your request to have only male staff members assigned to care for you." This response shows that the nurse is respecting the client's wishes and taking appropriate action to address their concerns.
Option B is incorrect because it is not within the nurse's scope of practice to arrange for a specific AP to provide care.
Option C is incorrect because it does not address the client's concerns or wishes.
Option D is incorrect because it may be perceived as confrontational and does not address the client's concerns in a respectful and professional manner.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
