A nurse is triaging clients following a mass casualty event. Which of the following clients should the nurse assess first?
A client who has a small circular partial-thickness burn of the left calf.
A client who has severe respiratory stridor and a deviated trachea.
A client who has a splinted open fracture of the left medial malleolus.
A client who has a massive head injury and is experiencing seizures.
The Correct Answer is B
Choice A reason: A Client Who Has a Small Circular Partial-Thickness Burn of the Left Calf
A small circular partial-thickness burn of the left calf is considered a minor injury in the context of a mass casualty event. This type of injury does not pose an immediate threat to life and can be managed after more critical cases are addressed. In mass casualty triage, patients with minor injuries are often categorized as “green” or “minimal” and are treated last.
Choice B reason: A Client Who Has Severe Respiratory Stridor and a Deviated Trachea
A client with severe respiratory stridor and a deviated trachea should be assessed first. These symptoms indicate a potential airway obstruction, which is a life-threatening condition requiring immediate intervention. In mass casualty triage, patients with compromised airways are given the highest priority and are categorized as “red” or “immediate” because their condition is critical and requires urgent medical attention.
Choice C reason: A Client Who Has a Splinted Open Fracture of the Left Medial Malleolus
A splinted open fracture of the left medial malleolus is a serious injury but not immediately life-threatening if properly splinted. This client would be categorized as “yellow” or “delayed” in mass casualty triage, meaning they require medical attention but can wait until more critical patients are stabilized.
Choice D reason: A Client Who Has a Massive Head Injury and Is Experiencing Seizures
A client with a massive head injury and experiencing seizures is in a critical condition. However, in the context of mass casualty triage, the immediate priority is to secure the airway, breathing, and circulation. While this client is in dire need of medical attention, the presence of severe respiratory stridor and a deviated trachea in another client takes precedence due to the immediate threat to life.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A reason: Ulnar Deviation
Ulnar deviation, or the bending of the fingers towards the ulna (the outer bone of the forearm), is more commonly associated with rheumatoid arthritis rather than osteoarthritis. Rheumatoid arthritis typically affects the joints symmetrically and can lead to deformities such as ulnar deviation due to chronic inflammation.
Choice B reason: Symmetric Joints Affected
Symmetric joint involvement is characteristic of rheumatoid arthritis, not osteoarthritis. Osteoarthritis usually affects joints asymmetrically, meaning it can affect one joint more than the other. It commonly affects weight-bearing joints such as the knees, hips, and spine.
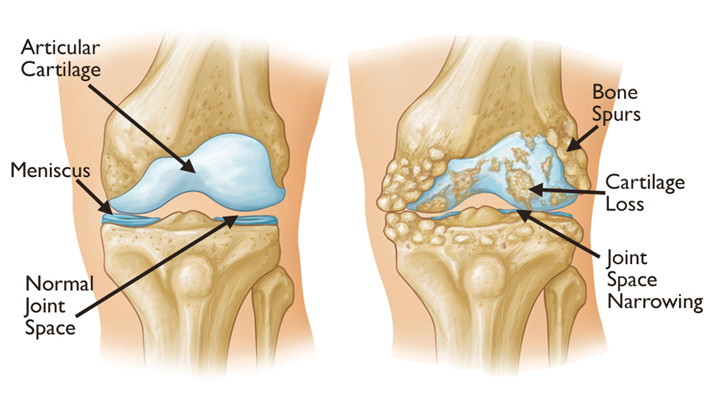
Choice C reason: Pain Worsens with Activity
Pain that worsens with activity is a hallmark symptom of osteoarthritis. This condition is caused by the breakdown of cartilage in the joints, leading to pain and stiffness, especially after physical activity. The pain typically improves with rest but can become more persistent as the disease progresses.
Choice D reason: Weight Loss
Weight loss is not a typical manifestation of osteoarthritis. In fact, being overweight or obese is a risk factor for developing osteoarthritis, particularly in weight-bearing joints. Weight management is often recommended to help reduce the stress on affected joints and alleviate symptoms.
Correct Answer is B
Explanation
Choice A reason:
Health care provider: While health care providers, such as doctors, have extensive knowledge about medications and their uses, they may not always have the most up-to-date information on specific drug compatibilities. Pharmacists specialize in medications and are more likely to have immediate access to detailed compatibility data.
Choice B reason:
Hospital pharmacist: Pharmacists are the primary resource for information on drug compatibility. They have access to comprehensive databases and resources that provide detailed information on drug interactions and compatibility. Consulting the hospital pharmacist ensures that the nurse receives accurate and current information regarding the safe administration of ampicillin and gentamicin sulfate.
Choice C reason:
Nurse manager: Nurse managers oversee nursing staff and ensure that patient care standards are met. While they have a broad knowledge of clinical practices, they may not have the specific expertise or resources to provide detailed information on drug compatibility.
Choice D reason:
Medication sales representative: Medication sales representatives are knowledgeable about the products they promote, but their primary role is to market medications. They may not have the comprehensive and unbiased information needed to determine drug compatibility. It is always best to consult a pharmacist for this type of information.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
