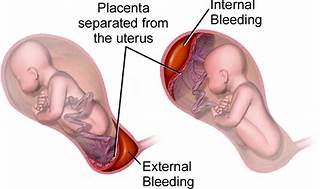
A nurse is reinforcing teaching with a client who is at 34 weeks of gestation and at risk for placental abruption. Does the nurse recognize that which of the following is the most common risk factor for a placental abruption?
Maternal hypertension.
Maternal cocaine use.
Maternal cigarette smoking.
Maternal battering.
The Correct Answer is A
The correct answer is choice A, Maternal hypertension.
Choice A rationale:
Maternal hypertension is widely recognized as the most common risk factor for placental abruption. High blood pressure can cause the placenta to detach from the uterine wall, leading to abruption. In summary, while all the listed factors can contribute to the risk of placental abruption, maternal hypertension stands out as the most common cause, supported by multiple health sources. It’s important for nurses to recognize and manage hypertension in pregnant clients to minimize the risk of this serious complication.
Choice B rationale:
While maternal cocaine use is a significant risk factor for placental abruption due to its vasoconstrictive effects, which can compromise the placental blood flow, it is not as common as maternal hypertension.
Choice C rationale:
Maternal cigarette smoking is also a risk factor for placental abruption. Smoking can lead to a variety of complications in pregnancy, including placental problems, but again, it is less common than hypertension as a cause for abruption.
Choice D rationale:
Maternal battering can lead to trauma which may result in placental abruption. However, it is not considered the most common risk factor when compared to maternal hypertension.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A rationale :
The correct answer is A. Calcium gluconate. The nurse should administer calcium gluconate in this situation because the client's respiratory rate is 8/min, which indicates respiratory depression. Magnesium sulfate is known to cause respiratory depression as a side effect, and calcium gluconate is the antidote for magnesium sulfate toxicity. Calcium gluconate works by antagonizing the effects of magnesium on the neuromuscular junction and restoring normal respiratory function. Prompt administration of calcium gluconate can help reverse respiratory depression and prevent further complications.
Choice B rationale
Naloxone. Naloxone is not the correct choice in this scenario. Naloxone is an opioid antagonist and is used to reverse the effects of opioids in cases of opioid overdose. Since the client is receiving magnesium sulfate, which is not an opioid, naloxone would not be effective in reversing the respiratory depression caused by magnesium sulfate. Administering naloxone in this situation would not address the underlying cause and may not improve the client's condition.
Choice C rationale
Flumazenil. Flumazenil is not the correct choice in this situation. Flumazenil is a benzodiazepine antagonist and is used to reverse the effects of benzodiazepines in cases of benzodiazepine overdose. Since the client is not receiving benzodiazepines but rather magnesium sulfate, flumazenil would not be effective in treating the respiratory depression caused by magnesium sulfate. Using flumazenil in this context would not be appropriate and could potentially lead to adverse effects.
Choice D rationale
Protamine sulfate. Protamine sulfate is not the correct choice in this scenario. Protamine sulfate is an antidote for heparin overdose, not for magnesium sulfate toxicity. It works by neutralizing the effects of heparin and preventing further anticoagulation. Since the client's issue is respiratory depression caused by magnesium sulfate, administering protamine sulfate would not be helpful and would not address the primary problem.
Correct Answer is A
Explanation
Choice A rationale:
The nurse should recommend the client to increase cellulose and fluid in the diet. Cellulose is a type of fiber found in fruits, vegetables, and whole grains. Increasing fiber intake can help alleviate constipation by adding bulk to the stool and promoting regular bowel movements. Additionally, the recommendation to increase fluid intake complements the effect of fiber, as it softens the stool, making it easier to pass through the intestines. This combination of increased cellulose and fluid intake is a safe and natural way to address constipation during pregnancy without the need for medication or invasive interventions.
Choice B rationale:
Regular use of glycerine suppositories is not the best recommendation for pregnant clients experiencing constipation. Suppositories are inserted into the rectum to stimulate bowel movements and should only be used sparingly when other methods have failed. Pregnant individuals may have increased sensitivity, and it's essential to avoid unnecessary procedures or potential discomfort.
Choice C rationale:
Regular use of a laxative is also not the most suitable recommendation for a pregnant client with constipation. While laxatives can provide relief, they may lead to dependency and might have adverse effects on the developing fetus. It is best to explore safer and more natural methods before resorting to laxative use during pregnancy.
Choice D rationale:
Maintenance of good posture is essential during pregnancy for various rationales, but it is not a specific solution for constipation. While maintaining good posture can help alleviate back pain and other discomforts, it does not directly address the issue of constipation.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
