A nurse is providing teaching to a client who is at 32 weeks of gestation and is experiencing stress incontinence. Which of the following information should the nurse include in the teaching? (Select all that apply.)
Decrease dietary fiber.
Practice Kegel exercises.
Restrict daily fluid intake.
Reduce caffeine intake.
Avoid daily exercise.
Correct Answer : B,D
Choice A rationale:
This would be incorrect advice. Increasing dietary fiber is commonly recommended during pregnancy to prevent constipation, but it does not address stress incontinence.
Choice B rationale:
This is a correct choice. Kegel exercises are beneficial during pregnancy to strengthen the pelvic floor muscles, which can help manage stress incontinence.
Choice C rationale:
This would be incorrect advice. Restricting daily fluid intake during pregnancy is generally not recommended as it can lead to dehydration and is unlikely to improve stress incontinence.
Choice D rationale:
This is another correct choice. Caffeine is a bladder irritant and can worsen stress incontinence, so reducing caffeine intake can be helpful.
Choice E rationale:
This would be incorrect advice. Regular exercise during pregnancy is generally encouraged unless there are specific medical reasons to avoid it. Avoiding daily exercise is not the appropriate approach to manage stress incontinence.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice C rationale:
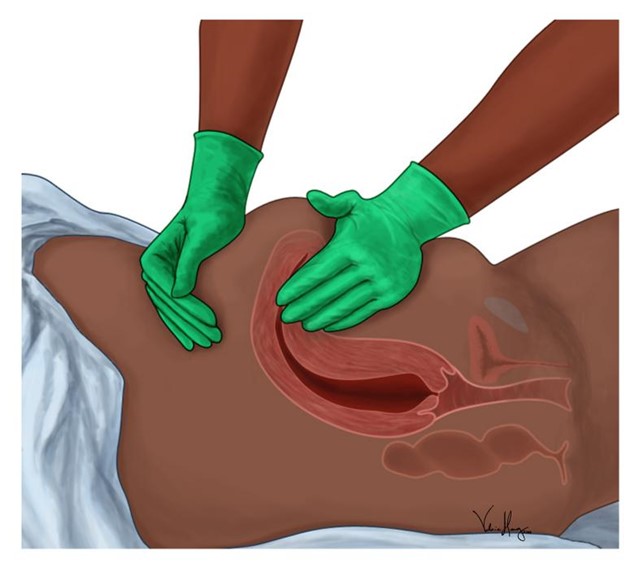
The nurse should first massage the client's fundus to address the excessive vaginal bleeding. Massaging the fundus helps the uterus contract and prevents further bleeding. Excessive postpartum bleeding may indicate uterine atony, which is a leading cause of postpartum hemorrhage. The nurse should apply gentle pressure to the fundus to promote uterine contractions and reduce bleeding.
Choice A rationale:
Elevating the client's legs to a 30° angle (Trendelenburg position) is not the priority action in this situation. Fundal massage takes precedence because it directly addresses the cause of the excessive bleeding. While Trendelenburg position might be used in some situations to increase blood flow to vital organs, it is not the first-line intervention for postpartum bleeding.
Choice B rationale:
Inserting an indwelling urinary catheter is not the priority action for excessive vaginal bleeding. While monitoring urine output is essential, the immediate concern is controlling the bleeding by massaging the fundus.
Choice D rationale:
Initiating an infusion of oxytocin may be indicated if fundal massage alone is insufficient to control bleeding. However, massaging the fundus should be the first action taken to promote uterine contractions. Oxytocin can be administered afterward, if needed, under the direction of a healthcare provider.
Correct Answer is ["C","D","E"]
Explanation
The correct answers are C, D, E.
Choice A reason:
Performing a vaginal exam is contraindicated in placenta previa because it can disrupt the placenta and cause significant bleeding.
Choice B reason:
Monitoring fetal heart rate with an internal fetal monitor is not recommended as it involves a vaginal exam, which poses a risk of bleeding in placenta previa cases.
Choice C reason:
Frequently assessing maternal heart rate is important to detect any changes that could indicate maternal hemorrhage or other complications.
Choice D reason:
Initiating bed rest with bathroom privileges is advised to minimize the risk of bleeding and to ensure the safety of both the mother and the fetus.
Choice E reason:
Having oxygen equipment available is essential to manage potential fetal distress, which can occur with placenta previa.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
