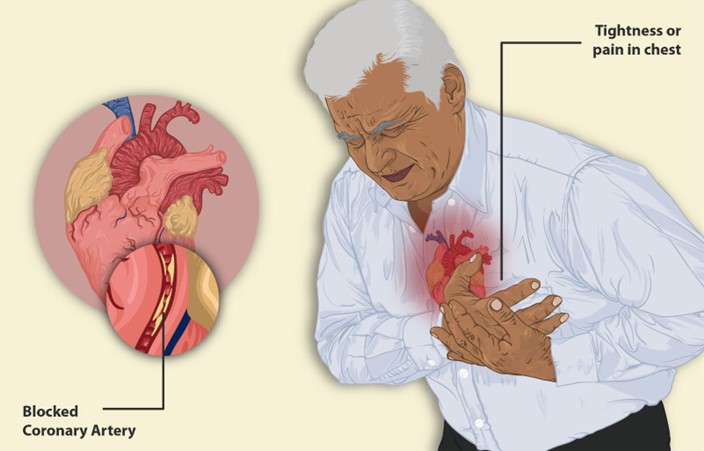
A nurse is providing teaching for a client who has a new diagnosis of angina pectoris. Which of the following information should the nurse include about anginal pain?
The pain usually lasts longer than 20 min.
The pain persists with rest and organic nitrates.
Pain can often be relieved by sitting up.
Exertion and anxiety can trigger the pain.
The Correct Answer is D
Choice A Reason: This is incorrect. Anginal pain usually lasts less than 20 min and subsides with rest or medication. Pain that lasts longer than 20 min may indicate a myocardial infarction.
Choice B Reason: This is incorrect. Anginal pain usually responds to rest and organic nitrates, such as nitroglycerin. Pain that does not improve with these measures may indicate unstable angina or a myocardial infarction.
Choice C Reason: This is incorrect. Anginal pain is not affected by the position of the client. Pain that is relieved by sitting up may indicate pericarditis or pleurisy.
Choice D Reason: This is correct. Anginal pain is caused by a temporary imbalance between the oxygen demand and supply of the myocardium. Factors that increase the oxygen demand, such as exertion, anxiety, cold, or heavy meals, can trigger anginal pain.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason: This is incorrect because droplet precautions are not sufficient to prevent the transmission of pneumonic plague. Droplet precautions are used to prevent the spread of infectious agents that are expelled through coughing, sneezing, or talking and travel only a short distance in the air. Droplet precautions include wearing a surgical mask, gown, and gloves, and placing the client in a private room or with a roommate who has the same infection.
Choice B Reason: This is incorrect because administering an antitoxin is not an intervention for pneumonic plague. An antitoxin is a substance that neutralizes the effects of a toxin produced by a microorganism. Pneumonic plague is not caused by a toxin, but by a bacterial infection.
Choice C Reason: This is correct because initiating airborne precautions is an intervention for pneumonic plague. Airborne precautions are used to prevent the spread of infectious agents that can remain suspended in the air and travel over long distances. Pneumonic plague is a severe and potentially fatal infection caused by the bacterium Yersinia pestis, which can be transmited through respiratory droplets or aerosols. Airborne precautions are used to prevent the spread of infectious agents that can remain suspended in the air and travel over long distances. Airborne precautions include wearing a respirator or N95 mask, placing the client in a negative-pressure room with an air filtration system, and limiting visitors and staff contact.
Choice D Reason: This is incorrect because destroying the linens after use is not an intervention for pneumonic plague. Linens that are contaminated with body fluids or secretions should be handled with gloves and placed in leak-proof bags for laundering or disposal, but they do not need to be destroyed.

Correct Answer is B
Explanation
Choice A Reason: This is incorrect. Widening pulse pressure is not a sign of hypovolemic shock, but rather of increased intracranial pressure or aortic regurgitation. Hypovolemic shock causes narrowing pulse pressure due to decreased stroke volume and increased peripheral resistance.
Choice B Reason: This is correct. Increased heart rate is a sign of hypovolemic shock, as the body tries to compensate for the decreased blood volume and cardiac output by increasing the heart rate and contractility.
Choice C Reason: This is incorrect. Increased deep tendon reflexes are not a sign of hypovolemic shock, but rather of hyperreflexia or tetany. Hypovolemic shock causes decreased deep tendon reflexes due to reduced perfusion and oxygenation of the muscles and nerves.
Choice D Reason: This is incorrect. Pulse oximetry 96% is not a sign of hypovolemic shock, but rather of normal oxygen saturation. Hypovolemic shock causes decreased pulse oximetry due to hypoxia and impaired gas exchange.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
