A nurse in the emergency department is monitoring a client who has a cervical spinal cord injury from a fall. The nurse should monitor the client for which of the following complications? (Select all that apply.)
Weakened gag reflex
Hyperthermia
Absence of bowel sounds
Paralysis
Polyuria
Hypotension
Correct Answer : A,C,D,F
Choice A: A cervical spinal cord injury can impair the function of cranial nerves, leading to a weakened gag reflex and an increased risk of aspiration.
Choice B: Patients with spinal cord injuries are more likely to experience poikilothermia (difficulty regulating body temperature), but this often results in hypothermia, not hyperthermia, due to the loss of autonomic temperature control.
Choice C: Spinal shock, which often follows a spinal cord injury, can cause decreased or absent bowel sounds due to a temporary loss of autonomic function and decreased peristalsis.
Choice D: Depending on the level and severity of the injury, paralysis can occur, affecting motor function below the injury site. A cervical spinal cord injury may lead to quadriplegia (tetraplegia).
Choice E: Clients with spinal cord injuries are more likely to experience urinary retention, rather than polyuria, due to loss of bladder control and autonomic dysfunction. A foley catheter may be needed initially, followed by intermittent catheterization.
Choice F: Neurogenic shock, a potential complication of cervical spinal cord injuries, can cause hypotension due to the loss of sympathetic nervous system control over blood vessel tone, leading to vasodilation and bradycardia.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
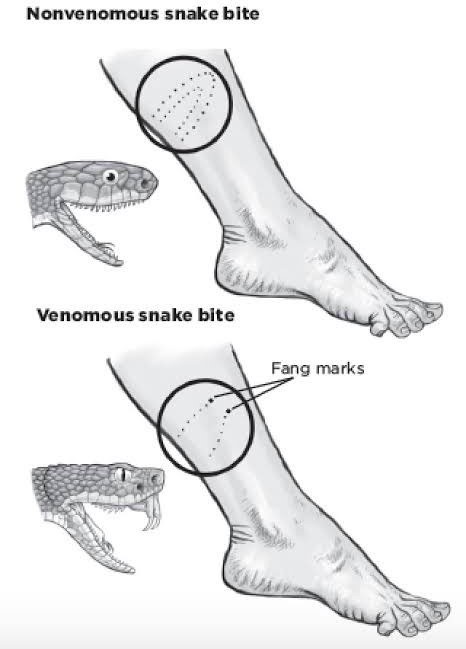
Choice A Reason: This is correct. The nurse should remove both of the elastic bandages from the leg, as they can impair blood flow and increase tissue damage. The nurse should also elevate the leg and keep it immobile to reduce venom absorption.
Choice B Reason: This is incorrect. The nurse should not discharge the client, as they may develop serious complications from the snake bite, such as swelling, bleeding, infection, or shock. The client should be monitored closely and treated accordingly.
Choice C Reason: This is incorrect. The nurse should not obtain a prescription for the appropriate anti-venom, as this is not within their scope of practice. The nurse should notify the physician and provide supportive care until the physician arrives and decides whether to administer anti-venom or not.
Choice D Reason: This is incorrect. The nurse should not obtain a prescription for pain medication, as this may mask the symptoms of venom toxicity or cause adverse reactions with anti-venom. The nurse should use non- pharmacological methods to relieve pain, such as ice packs or distraction.
Correct Answer is C
Explanation
Choice A: Removing the elastic bandages is not recommended. These bandages help slow the spread of venom by compressing the lymphatic vessels. Removing them could worsen the envenomation.
Choice B: This is incorrect. The nurse should not discharge the client, as they may develop serious complications from the snake bite, such as swelling, bleeding, infection, or shock. The client should be monitored closely and treated accordingly.
Choice C: This is the correct action. Antivenom treatment is crucial for serious snake envenomation. The sooner it can be administered, the better the outcome.
Choice D: While pain management is important, it is not the priority in this situation. Antivenom takes precedence over pain medication.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
