A nurse in the emergency department is assessing a client who has internal injuries from a car crash. The client is disoriented to time and place, diaphoretic, and his lips are cyanotic. The nurse should anticipate which of the following findings as an indication of hypovolemic shock?
Widening pulse pressure
Increased heart rate
Increased deep tendon reflexes
Pulse oximetry 96%
The Correct Answer is B
Choice A Reason: This is incorrect. Widening pulse pressure is not a sign of hypovolemic shock, but rather of increased intracranial pressure or aortic regurgitation. Hypovolemic shock causes narrowing pulse pressure due to decreased stroke volume and increased peripheral resistance.
Choice B Reason: This is correct. Increased heart rate is a sign of hypovolemic shock, as the body tries to compensate for the decreased blood volume and cardiac output by increasing the heart rate and contractility.
Choice C Reason: This is incorrect. Increased deep tendon reflexes are not a sign of hypovolemic shock, but rather of hyperreflexia or tetany. Hypovolemic shock causes decreased deep tendon reflexes due to reduced perfusion and oxygenation of the muscles and nerves.
Choice D Reason: This is incorrect. Pulse oximetry 96% is not a sign of hypovolemic shock, but rather of normal oxygen saturation. Hypovolemic shock causes decreased pulse oximetry due to hypoxia and impaired gas exchange.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A: Cold and numb sensation distal to the fistula site is a possible indication of venous insufficiency. Venous insufficiency is a condition in which the veins have difficulty returning blood from the limbs to the heart, resulting in blood pooling and reduced perfusion. A new arteriovenous fistula can cause increased blood flow through the artery and decreased blood flow through the vein, leading to venous insufficiency. This can manifest as coldness, numbness, tingling, or cyanosis in the fingers or hand below the fistula site.
Choice B: A raised red rash around the fistula site is not a possible indication of venous insufficiency. A raised red rash around the fistula site can indicate an allergic reaction, an infection, or an inflammation of the skin or subcutaneous tissue. The nurse should assess the rash for size, shape, color, texture, temperature, and drainage, and report any signs of infection or inflammation, such as fever, pus, or swelling.
Choice C: Pain in the right arm proximal to the fistula site is not a possible indication of venous insufficiency. Pain in the right arm proximal to the fistula site can indicate arterial insufficiency, which is a condition in which the arteries have difficulty delivering oxygen-rich blood to the tissues, resulting in ischemia and necrosis. Arterial insufficiency can be caused by atherosclerosis, thrombosis, embolism, or vasospasm. The nurse should assess the pain for location, intensity, duration, frequency, and quality, and report any signs of ischemia or necrosis, such as pallor, coolness, weak pulses, or ulceration.
Choice D: Foul-smelling drainage from the fistula site is not a possible indication of venous insufficiency. Foul-smelling drainage from the fistula site can indicate an infection of the fistula or surrounding tissue. The nurse should assess the drainage for color, odor, amount, and consistency, and report any signs of infection or sepsis, such as fever, chills, malaise, or hypotension.
Correct Answer is D
Explanation
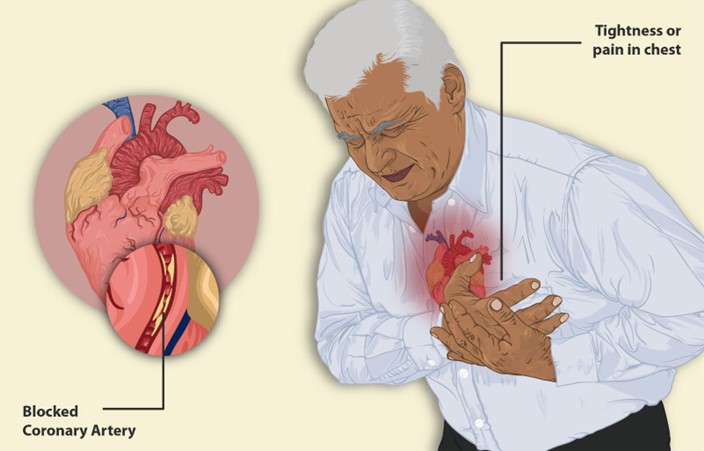
Choice A Reason: This is incorrect. Anginal pain usually lasts less than 20 min and subsides with rest or medication. Pain that lasts longer than 20 min may indicate a myocardial infarction.
Choice B Reason: This is incorrect. Anginal pain usually responds to rest and organic nitrates, such as nitroglycerin. Pain that does not improve with these measures may indicate unstable angina or a myocardial infarction.
Choice C Reason: This is incorrect. Anginal pain is not affected by the position of the client. Pain that is relieved by sitting up may indicate pericarditis or pleurisy.
Choice D Reason: This is correct. Anginal pain is caused by a temporary imbalance between the oxygen demand and supply of the myocardium. Factors that increase the oxygen demand, such as exertion, anxiety, cold, or heavy meals, can trigger anginal pain.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
