A nurse is providing teaching about nutrition to a client at her first prenatal visit. Which of the following statements by the nurse should be included in the teaching?
Vitamin E requirements decrease during pregnancy due to the increase in body fat.
Prenatal vitamins will meet your need for increased folic acid during pregnancy.
You will need to double your intake of protein during pregnancy.
You will need to increase your intake of calcium during pregnancy.
The Correct Answer is B
Choice A: Vitamin E requirements do not decrease during pregnancy due to the increase in body fat. Vitamin E is a fat-soluble vitamin that acts as an antioxidant and protects cell membranes from oxidative damage. The recommended dietary allowance (RDA) for vitamin E during pregnancy is 15 mg/day, which is the same as for non-pregnant women.
Choice B: Prenatal vitamins will meet your need for increased folic acid during pregnancy. Folic acid is a water-soluble vitamin that is essential for DNA synthesis and cell division. Folic acid deficiency can cause neural tube defects in the fetus, such as spina bifida and anencephaly. The RDA for folic acid during pregnancy is 600 mcg/day, which can be obtained from prenatal vitamins and fortified foods.
Choice C: You will not need to double your intake of protein during pregnancy. Protein is a macronutrient that provides amino acids for tissue growth and repair. The RDA for protein during pregnancy is 1.1 g/kg/day, which is only slightly higher than for non-pregnant women (0.8 g/kg/day).
Choice D: You will not need to increase your intake of calcium during pregnancy. Calcium is a mineral that is important for bone health and muscle contraction. Calcium absorption and retention are enhanced during pregnancy, so there is no need to increase the intake above the RDA of 1000 mg/day for women aged 19 to 50 years.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["415"]
Explanation
To calculate the amount of NG drainage, the nurse should subtract the amount of irrigation fluid from the amount of fluid in the NG canister. The irrigation fluid is not part of the drainage, but rather a way to keep the NG tube patent and prevent clogging.
The amount of irrigation fluid is 30 mL x 2 = 60 mL.
The amount of fluid in the NG canister is 475 mL.
Therefore, the amount of NG drainage is 475 mL - 60 mL = 415 mL.
The answer should be rounded to the nearest whole number and use a leading zero if it applies. Do not use a trailing zero.
Therefore, the final answer is 415 mL.
Correct Answer is A
Explanation
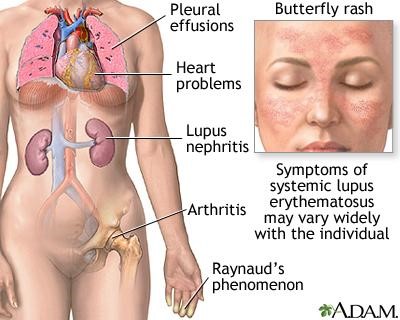
Choice A Reason: This is correct because this response provides realistic and supportive advice for a woman who wants to have a baby with lupus. Lupus is an autoimmune disease that causes inflammation and damage to various organs and tissues. Lupus can affect fertility and pregnancy outcomes, such as increasing the risk of miscarriage, preterm delivery, preeclampsia, or neonatal lupus. Therefore, it is important for the woman to have her lupus under control before conceiving and to consult with her doctor about her treatment plan and prenatal care.
Choice B Reason: This is incorrect because this response is discouraging and insensitive for the woman who wants to have a baby with lupus. Lupus does not necessarily prevent a woman from having a healthy pregnancy and a healthy baby, as long as she follows her doctor's recommendations and monitors her condition closely. The nurse should respect the woman's reproductive choices and provide information and support.
Choice C Reason: This is incorrect because this response is inaccurate and misleading for the woman who wants to have a baby with lupus. Lupus can have various effects on pregnancy, such as causing flares or complications that can affect both the mother and the baby. The nurse should educate the woman about the possible risks and benefits of pregnancy with lupus and help her prepare for any challenges.
Choice D Reason: This is incorrect because this response is vague and alarming for the woman who wants to have a baby with lupus. Lupus treatment may or may not change during pregnancy, depending on the type and severity of lupus, the medications used, and the stage of pregnancy. The nurse should explain the rationale and safety of any medication changes and address any concerns or questions that the woman may have.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
