A nurse is preparing to turn a client who is obese following a spinal fusion. The nurse should plan to use which of the following techniques to turn this client?
Draw sheet
Log roll
Sliding board
Hoyer lift
The Correct Answer is B
Choice A reason:
Draw sheet: A draw sheet can be used to assist in repositioning a patient, but it is not the most effective method for turning a client who has undergone spinal fusion. The primary concern is to maintain spinal alignment, which is best achieved through the log roll technique.
Choice B reason:
Log roll: The log roll technique is the preferred method for turning patients who have had spinal surgery. This technique involves moving the patient as a single unit, keeping the spine in alignment to prevent any twisting or bending that could disrupt the surgical site. It is especially important for obese patients to ensure that the spine remains stable during movement.
Choice C reason:
Sliding board: A sliding board is typically used to assist with transfers from one surface to another, such as from a bed to a wheelchair. It is not suitable for turning a patient in bed, particularly one who has had spinal surgery.
Choice D reason:
Hoyer lift: A Hoyer lift is a mechanical device used to lift and transfer patients who are unable to move themselves. While it can be useful for transferring patients, it is not designed for turning patients in bed and does not provide the necessary support to maintain spinal alignment during a turn.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A reason:
WBC count: An elevated white blood cell (WBC) count is a common indicator of infection. The body produces more white blood cells to fight off infections, making this a key marker for identifying infections in patients with pressure ulcers. Monitoring WBC count helps in assessing the presence and severity of an infection, guiding appropriate treatment.
Choice B reason:
BUN: Blood urea nitrogen (BUN) levels are used to assess kidney function and hydration status. Elevated BUN levels can indicate dehydration or kidney dysfunction but are not specific indicators of infection. While important for overall health assessment, BUN is not directly related to detecting infections in pressure ulcers.
Choice C reason:
Potassium: Potassium levels are crucial for maintaining normal cellular function, particularly in the heart and muscles. Abnormal potassium levels can indicate issues such as kidney dysfunction or electrolyte imbalances but do not specifically indicate infection. Monitoring potassium is important for overall health but not for diagnosing infections in pressure ulcers.
Correct Answer is B
Explanation
Choice A reason:
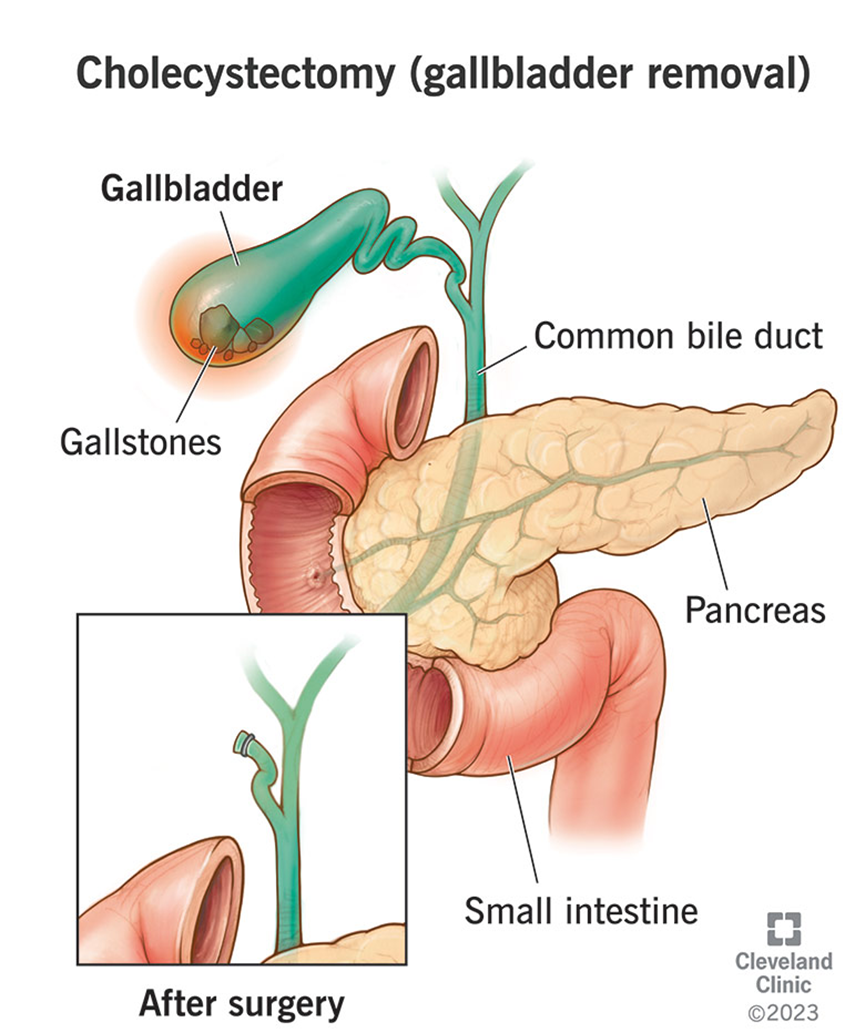
Supported Sims: The Supported Sims position involves lying on one side with the lower arm behind the back and the upper thigh flexed. This position is not typically recommended for postoperative cholecystectomy patients as it does not provide optimal support for breathing and comfort.
Choice B reason:
Semi-Fowler’s: The Semi-Fowler’s position, where the head of the bed is elevated to about 30-45 degrees, is ideal for postoperative cholecystectomy patients. This position helps facilitate breathing, reduces the risk of aspiration, and promotes comfort by reducing tension on the abdominal muscles.
Choice C reason:
Dorsal recumbent: The Dorsal recumbent position involves lying flat on the back with knees bent and feet flat on the bed. While this position can be used for certain procedures, it is not the most comfortable or beneficial for postoperative cholecystectomy patients as it can increase abdominal pressure and discomfort.
Choice D reason:
Prone: The Prone position, where the patient lies flat on their stomach, is not suitable for postoperative cholecystectomy patients. This position can cause discomfort and does not support optimal breathing or reduce abdominal tension.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
