A nurse is preparing to administer an osmotic diuretic IV to a client with increased intracranial pressure. Which of the following should the nurse identify as the purpose of the medication?
Reduce edema of the brain.
Increase cell size in the brain.
Expand extracellular fluid volume.
Provide fluid hydration.
The Correct Answer is A
Choice A Reason: This is correct because an osmotic diuretic, such as mannitol, works by creating an osmotic gradient that draws fluid from the brain tissue into the blood vessels, thereby reducing cerebral edema and intracranial pressure.
Choice B Reason: This is incorrect because an osmotic diuretic would decrease, not increase, the cell size in the brain by removing fluid from the intracellular space.
Choice C Reason: This is incorrect because an osmotic diuretic would decrease, not expand, the extracellular fluid volume by increasing the urine output and excreting excess fluid from the body.
Choice D Reason: This is incorrect because an osmotic diuretic would not provide fluid hydration, but rather cause fluid loss and dehydration.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason: This is incorrect because a client who is post-CABG and has high cholesterol is not in immediate danger, as atorvastatin is a long-term medication that lowers cholesterol and prevents cardiovascular complications.
Choice B Reason: This is incorrect because a client who has pneumonia and a slightly elevated WBC count is not in immediate danger, as piperacillin is an antibiotic that treats bacterial infections.
Choice C Reason: This is correct because a client who has renal failure and a high serum potassium level is in immediate danger, as sodium polystyrene sulfonate is an emergency medication that lowers potassium and prevents cardiac arrhythmias.
Choice D Reason: This is incorrect because a client who has anemia and a mild hemoglobin deficiency is not in immediate danger, as epoetin alfa is a long-term medication that stimulates red blood cell production and improves oxygen delivery.
Correct Answer is D
Explanation
Choice A Reason: This is incorrect because administering a nitrate antihypertensive is not the first action, as it may cause a rapid drop in blood pressure and worsen the client's condition.
Choice B Reason: This is incorrect because obtaining the client's heart rate is not the first action, as it does not address the cause of autonomic dysreflexia or relieve the symptoms.
Choice C Reason: This is incorrect because assessing the client for bladder distention is not the first action, as it may take time and delay the treatment of autonomic dysreflexia.
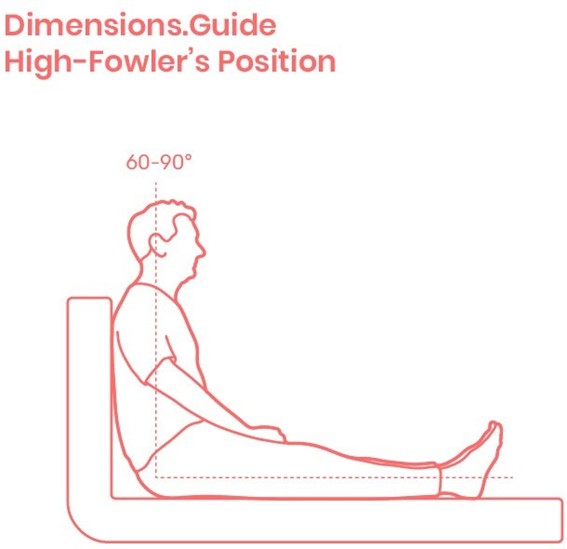
Choice D Reason: This is correct because placing the client in a high-Fowler's position is the first action, as it lowers the blood pressure by promoting venous return and reducing cardiac preload.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
