A nurse is planning care for a full-term newborn who is receiving phototherapy. Which of the following actions should the nurse include in the plan of care?
Keep the newborn supine throughout treatment.
Dress the newborn in lightweight clothing.
Measure the newborn's temperature every 8 hours.
Avoid using lotion or ointment on the newborn's skin.
The Correct Answer is D
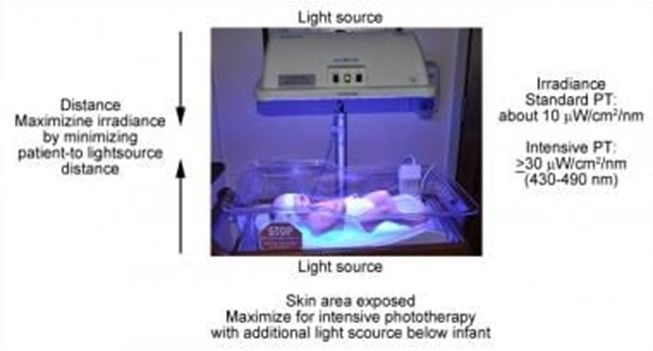
Phototherapy is a treatment that uses light to lower the level of bilirubin in the blood of newborns who have jaundice. Jaundice is a condition that causes yellowing of the skin and eyes due to high levels of bilirubin, a waste product that is normally removed by the liver. Phototherapy helps the body break down and eliminate bilirubin through urine and stool¹.
Phototherapy can be done at home or in the hospital, depending on the severity of jaundice and the type of light used. The most common types of light are fluorescent lamps, halogen lamps, or light-emitting diodes (LEDs). The light can be delivered through overhead units, fiber-optic blankets, or fiber-optic pads. The light should cover as much of the newborn's skin as possible, except for the eyes and genitals¹².
The nurse should follow certain guidelines when caring for a newborn who is receiving phototherapy, such
as:
- Monitor the newborn's temperature, hydration, weight, and urine and stool output regularly
- Protect the newborn's eyes with eye patches or goggles to prevent eye damage
- Turn the newborn every 2 to 4 hours to expose different parts of the body to the light
- Feed the newborn frequently to prevent dehydration and promote bilirubin excretion
- Check the newborn's skin color and bilirubin level periodically to evaluate the effectiveness of
phototherapy
- Provide emotional support and education to the parents about jaundice and phototherapy
One of the important guidelines is to avoid using lotion or ointment on the newborn's skin during phototherapy. This is because lotion or ointment can block the light from reaching the skin and reduce the effectiveness of phototherapy. Lotion or ointment can also cause skin irritation, rash, or burns if they react with the light. The newborn's skin should be clean and dry before phototherapy¹²³.
The other options are not actions that the nurse should include in the plan of care:
- a) Keep the newborn supine throughout treatment. This is not correct because keeping the newborn in one position can limit the exposure of different parts of the body to the light and reduce the effectiveness of phototherapy. The nurse should turn the newborn every 2 to 4 hours to expose different parts of the body to the light¹².
- b) Dress the newborn in lightweight clothing. This is not correct because dressing the newborn in clothing can block the light from reaching the skin and reduce the effectiveness of phototherapy. The newborn should be undressed except for a diaper during phototherapy¹².
- c) Measure the newborn's temperature every 8 hours. This is not correct because measuring the newborn's temperature every 8 hours may not be frequent enough to detect any changes in temperature that may occur during phototherapy. Phototherapy can cause overheating or hypothermia in newborns, depending on the type and intensity of light used. The nurse should monitor the newborn's temperature more often, such as every 2 to 4 hours, and adjust the room temperature or use blankets as needed¹².
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
This is the action that the nurse should take after recognizing an early deceleration of the fetal heart rate tracing. Early decelerations are symmetrical decreases and return-to-normal linked to uterine contractions¹. The decrease in heart rate occurs gradually, and the nadir of the deceleration occurs at the same time as the peak of the uterine contraction³. Early decelerations are caused by compression of the fetus's head during a uterine contraction, which can stimulate the vagus nerve and cause a decrease in the fetal heart rate⁴. Early decelerations are nothing to be alarmed about¹. They are considered normal and benign, as they do not affect fetal oxygenation or well-being³. Therefore, the nurse should continue to monitor the client and the fetal heart rate tracing and document the findings.
The other options are not correct because they are not appropriate actions for early decelerations.
a) Assist the client to lay on her right side.
This is not an appropriate action for early decelerations, as they are not caused by maternal position or uteroplacental insufficiency. Changing the maternal position may help improve fetal oxygenation and blood flow in cases of late or variable decelerations, which are signs of fetal distress¹. However, early decelerations do not indicate fetal distress and do not require any intervention.
c) Discontinue the oxytocin.
This is not an appropriate action for early decelerations, as they are not caused by oxytocin administration or uterine hyperstimulation. Oxytocin is a hormone that stimulates uterine contractions and can be used to induce or augment labor. However, excessive or prolonged use of oxytocin can cause uterine fatigue and reduce its ability to contract after delivery, leading to uterine atony and postpartum hemorrhage². Oxytocin can also cause late or variable decelerations, which are signs of fetal distress¹. However, early decelerations do not indicate fetal distress and do not require any intervention.
d) Administer oxygen at 8 L/min per mask.
This is not an appropriate action for early decelerations, as they are not caused by fetal hypoxia or acidosis. Oxygen administration may help improve fetal oxygenation and blood flow in cases of late or variable decelerations, which are signs of fetal distress¹. However, early decelerations do not indicate fetal distress and do not require any intervention.
Correct Answer is D
Explanation
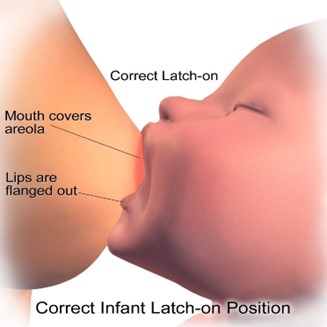
Sore nipples are a common problem for breastfeeding mothers, especially in the first few days or weeks after delivery. They can cause pain, discomfort, and frustration, and may interfere with breastfeeding success and satisfaction. The most common cause of sore nipples is poor latch, which means that the newborn does not attach to the breast correctly and does not suckle effectively. Poor latch can result from various factors, such as improper positioning, tongue-tie, inverted or flat nipples, engorgement, or thrush.
The nurse should assess the newborn's latch while breastfeeding to identify and correct any problems that may cause sore nipples. The nurse should observe the following signs of a good latch:
- The newborn's mouth is wide open and covers most of the areola (the dark area around the nipple).
- The newborn's chin and nose touch the breast, and the cheeks are rounded and not dimpled.
- The newborn's tongue is visible under the lower lip and curls around the breast.
- The newborn's lips are flanged outwards and not tucked inwards.
- The newborn's jaw moves rhythmically and smoothly, and swallowing sounds are audible.
- The mother feels a gentle tugging sensation on the nipple, but no pain or pinching.
The nurse should also teach the mother how to achieve a good latch by using different positions, supporting the breast with her hand, tickling the newborn's lower lip with her nipple, and bringing the newborn to the breast when their mouth is wide open. The nurse should also encourage the mother to seek help from a lactation consultant or a peer support group if she has persistent or severe nipple pain.
a) Instructing the client to wait 4 hours between daytime feedings is not an appropriate action for the nurse to take. This may reduce nipple soreness temporarily, but it can also cause breast engorgement, milk supply reduction, mastitis, or poor weight gain in the newborn. The nurse should advise the client to feed the newborn on demand, usually every 1.5 to 3 hours during the day and every 3 to 4 hours at night.
b) Offering supplemental formula between the newborn's feedings is not an appropriate action for the nurse to take. This may interfere with breastfeeding initiation and establishment, as it can reduce the mother's milk supply, confuse the newborn's sucking pattern, increase the risk of nipple preference or rejection, and expose the newborn to potential allergens or infections. The nurse should support exclusive breastfeeding for the first six months of life, unless there is a medical indication for supplementation.
c) Having the client limit the length of breastfeeding to 5 minutes per breast is not an appropriate action for the nurse to take. This may not be enough time for the newborn to get enough milk, especially the hindmilk that is richer in fat and calories. It may also prevent proper drainage of the breast and lead to engorgement or mastitis. The nurse should advise the client to let the newborn feed until they are satisfied and release the breast on their own, which may take 10 to 20 minutes per breast on average.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
