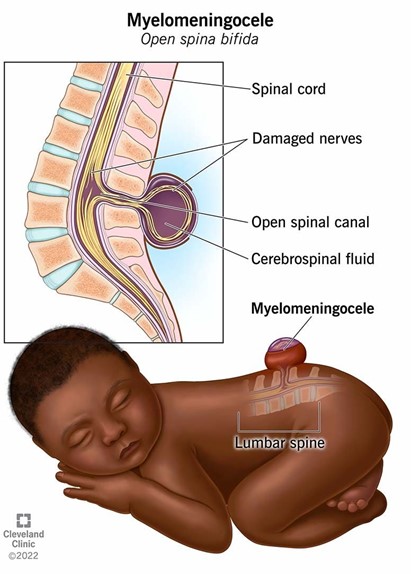
A nurse is planning care immediately following birth for a newborn who has a myelomeningocele that is leaking cerebrospinal fluid. Which of the following actions should the nurse include in the plan of care?
Cleanse the site with povidone-iodine.
Administer broad-spectrum antibiotics.
Prepare for surgical closure after 72 hours.
Monitor the rectal temperature every 4 hours.
The Correct Answer is B
A. Using povidone-iodine on the site of a myelomeningocele is not recommended as it can be irritating to the tissue and might not be safe for use on open neural tissue. The focus should be on preventing infection through other means.
B. Administering broad-spectrum antibiotics is crucial as the cerebrospinal fluid (CSF) leak increases the risk of infection, such as meningitis. Antibiotics help protect the newborn from potentially serious infections until surgical repair can be performed.
C. Surgical closure of a myelomeningocele is typically done as soon as possible, often within 24-48 hours after birth, to minimize the risk of infection and further damage to the exposed spinal cord.
D. While monitoring temperature is important, rectal temperature measurement is not recommended for a newborn with a myelomeningocele due to the risk of causing further complications. Axillary temperature measurement would be safer and less invasive.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
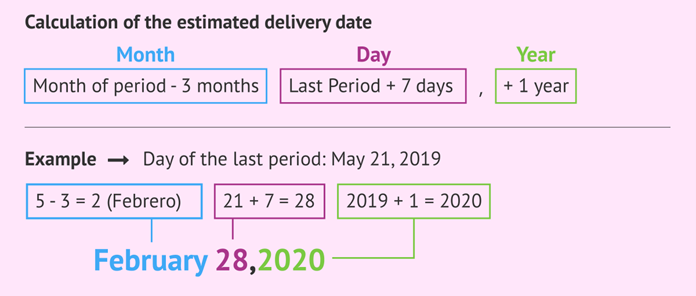
Nägele's Rule is a common method used to estimate the expected date of delivery (EDD) based on the first day of the client's last menstrual period (LMP). According to Nägele's Rule, you subtract 3 months from the LMP date and add 7 days, then adjust the year if necessary.
In this case, the first day of the client's last menstrual period was August 10. Subtracting 3 months gives us May 10. Adding 7 days gives us May 17. Therefore, the estimated date of delivery for this client is May 17.
Correct Answer is D
Explanation
Hemolytic disease of the newborn (HDN) is a condition that occurs when there is an incompatibility between the blood types of the mother and the baby. It causes the mother's immune system to produce antibodies that attack and destroy the baby's red blood cells, leading to anemia, jaundice, organ enlargement, and other complications¹.
One of the most common causes of HDN is Rh incompatibility. This happens when the mother is Rh negative and the baby is Rh positive. The Rh factor is a protein that can be present or absent on the surface of red blood cells. People who have the protein are Rh positive and people who do not have it are Rh negative
Rh incompatibility can cause HDN when the baby's Rh positive blood cells cross the placenta and enter the mother's bloodstream. This can happen during delivery, miscarriage, abortion, or invasive prenatal testing. The mother's immune system recognizes the baby's blood cells as foreign and produces antibodies against them. These antibodies can cross back to the baby's bloodstream and attack the baby's red blood cells, causing hemolysis (breakdown) and anemia².
HDN due to Rh incompatibility usually does not affect the first pregnancy, because the mother has not been exposed to Rh positive blood before and has not developed antibodies yet. However, it can affect subsequent pregnancies with Rh positive babies, because the mother has become sensitized and has antibodies ready to attack².
The other options are not causes of HDN:
a) The mother and the father are both Rh negative. This is not a cause of HDN because both parents have the same Rh factor and there is no incompatibility between them. The baby will also be Rh negative and will not trigger an immune response from the mother².
b) The mother and the father are both Rh positive. This is not a cause of HDN because both parents have the same Rh factor and there is no incompatibility between them. The baby will also be Rh positive and will not trigger an immune response from the mother².
c) The mother is Rh positive and the father is Rh negative. This is not a cause of HDN because the mother has a dominant Rh factor and will not produce antibodies against it. The baby will either be Rh positive or Rh negative, depending on whether they inherit the father's gene or not. In either case, the baby's blood type will not trigger an immune response from the mother².

Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
