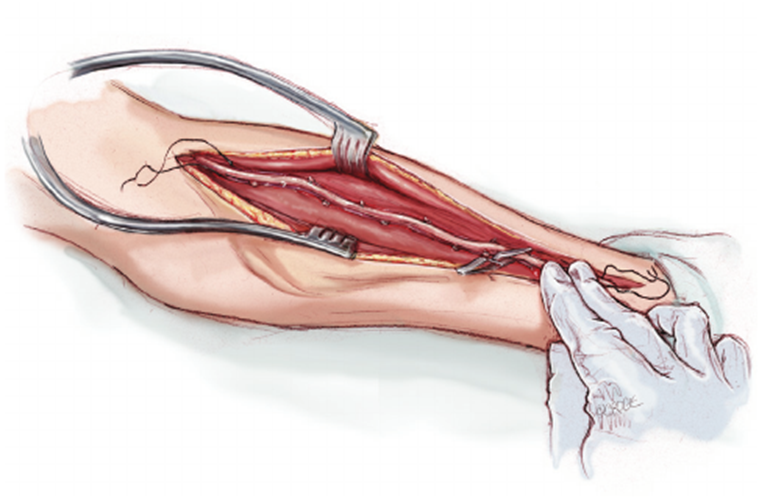
A nurse is planning care for a client who is postoperative following the insertion of an arteriovenous graft in their left forearm. Which of the following actions should the nurse include in the plan of care?
Check the pulse distal to the graft.
Keep the left forearm below the level of the heart.
Collect blood specimens from the graft.
Splint the left forearm to prevent damage to the graft.
The Correct Answer is A
Choice A reason: Checking the pulse distal to the graft is essential to ensure that the graft is patent and that there is adequate blood flow to the distal extremity. A palpable pulse indicates that the graft is functioning properly and not occluded. The absence of a pulse could signify a serious complication, such as thrombosis or stenosis, which requires immediate attention.
Choice B reason: Keeping the left forearm below the level of the heart is not recommended as it can increase venous pressure and swelling, potentially compromising graft function. The extremity should be kept at or above heart level to promote venous return and reduce the risk of edema.
Choice C reason: Collecting blood specimens from the graft is generally avoided to prevent damage to the graft. Blood draws can be performed from other sites to protect the integrity of the graft.
Choice D reason: Splinting the left forearm is not a standard postoperative care measure for an arteriovenous graft. While protecting the graft from injury is important, immobilization with a splint is not necessary and can impede mobility and circulation.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A reason: Drawing the regular insulin into the syringe first is correct. When mixing two types of insulin, the clear (regular) insulin should be drawn up before the cloudy (NPH) insulin to prevent contamination.
Choice B reason: Storing prefilled syringes with the needle pointed upward can cause air bubbles to move into the insulin, which can alter the dose when injected. The needle should be pointed downward.
Choice C reason: Shaking the NPH vial vigorously is not recommended as it can create air bubbles and affect the insulin dose. Instead, the vial should be gently rolled between the hands to mix the insulin.
Choice D reason: Inserting the needle at a 15-degree angle is incorrect for subcutaneous injections. A 90-degree angle is typically used unless the patient is very thin, in which case a 45-degree angle may be used.
Correct Answer is C
Explanation
Choice A reason : A blood pressure of 138/76 mm Hg is within the higher range of normal and is not typically considered an adverse effect of metoprolol, which is used to lower blood pressure.
Choice B reason : A temperature of 36.3°C (97.3°F) is within the normal range and is not an adverse effect of metoprolol.
Choice C reason : A heart rate of 48/min is considered bradycardia and can be an adverse effect of metoprolol, which is a beta-blocker that can slow down the heart rate.
Choice D reason : A respiratory rate of 10/min is on the lower end of the normal range but is not a typical adverse effect of metoprolol. However, if the patient shows signs of respiratory distress, it should be addressed.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
