A nurse is monitoring a client who is receiving a unit of packed red blood cells (RBCs) following surgery. Which of the following assessments is an indication that the client might be experiencing circulatory overload?
Bradycardia
Flushing
Vomiting
Dyspnea
The Correct Answer is D
Choice A reason: Bradycardia is not an indication of circulatory overload. Bradycardia is a slow heart rate, usually below 60 beats per minute. Circulatory overload causes the heart to work harder to pump the excess fluid in the blood vessels, which can result in tachycardia, or a fast heart rate, usually above 100 beats per minute.
Choice B reason: Flushing is not an indication of circulatory overload. Flushing is a reddening of the skin, usually due to increased blood flow or inflammation. Circulatory overload causes the blood vessels to constrict and increase the blood pressure, which can result in pallor, or a pale appearance of the skin.
Choice C reason: Vomiting is not an indication of circulatory overload. Vomiting is the forceful expulsion of stomach contents through the mouth, usually due to nausea, infection, or irritation. Circulatory overload does not affect the gastrointestinal system directly, although it may cause abdominal distension or ascites, which is the accumulation of fluid in the abdominal cavity.
Choice D reason: Dyspnea is an indication of circulatory overload. Dyspnea is the sensation of difficulty breathing, usually due to inadequate oxygen delivery to the tissues. Circulatory overload causes the excess fluid in the blood vessels to leak into the lungs, which can result in pulmonary edema, or the accumulation of fluid in the alveoli. This impairs the gas exchange and causes hypoxia, or low oxygen levels in the blood.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A reason: Bradycardia is not an adverse effect of diphenhydramine. Bradycardia is a slow heart rate, usually below 60 beats per minute. Diphenhydramine is an antihistamine that blocks the effects of histamine, a chemical that causes allergic reactions. Diphenhydramine does not affect the heart rate, although it may cause palpitations or irregular heartbeat in some cases.
Choice B reason: Constipation is an adverse effect of diphenhydramine. Constipation is a condition in which the bowel movements are infrequent, hard, or difficult to pass. Diphenhydramine has anticholinergic properties, which means it inhibits the activity of acetylcholine, a neurotransmitter that regulates the smooth muscle contraction in the gastrointestinal tract. Diphenhydramine can reduce the intestinal motility and cause constipation, as well as dry mouth, blurred vision, and urinary retention.
Choice C reason: Hypertension is not an adverse effect of diphenhydramine. Hypertension is a condition in which the blood pressure is abnormally high, usually above 140/90 mmHg. Diphenhydramine does not affect the blood pressure, although it may cause orthostatic hypotension, which is a sudden drop in blood pressure when changing positions from lying to standing. This can cause dizziness, fainting, or falls.
Choice D reason: Sedation is an adverse effect of diphenhydramine. Sedation is a state of reduced alertness, awareness, or responsiveness. Diphenhydramine can cross the blood-brain barrier and affect the central nervous system, causing drowsiness, fatigue, impaired coordination, and reduced mental performance. Diphenhydramine can also potentiate the effects of alcohol and other sedatives, such as benzodiazepines, opioids, or barbiturates. The nurse should advise the client to avoid driving, operating machinery, or performing other tasks that require attention and concentration while taking diphenhydramine.
Correct Answer is A
Explanation
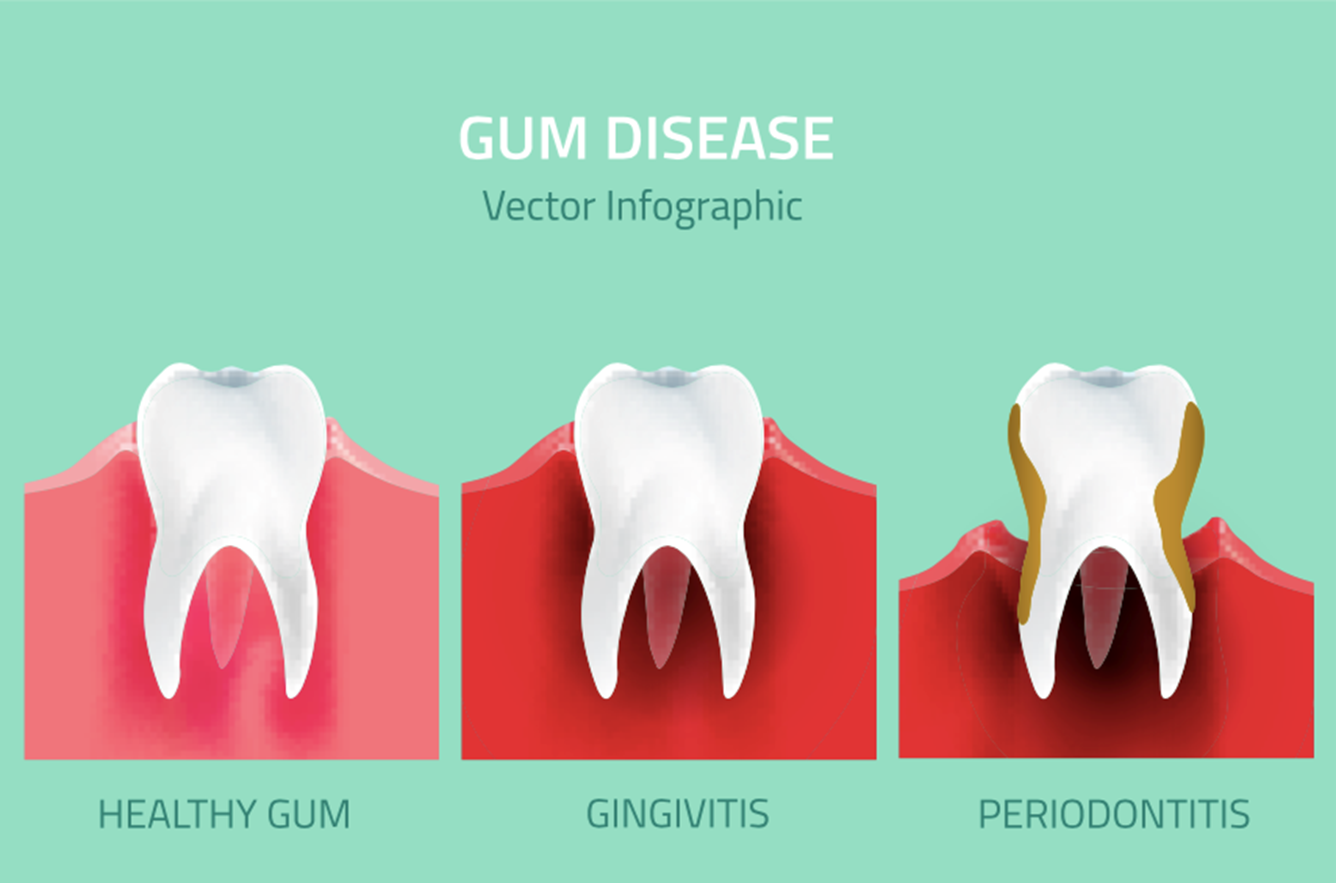
Choice A reason: Bleeding gums is a possible adverse effect of taking gingko biloba, as it may increase the risk of bleeding by inhibiting platelet aggregation and interfering with clotting factors. Gingko biloba may also interact with other medications that affect bleeding, such as anticoagulants, antiplatelets, or NSAIDs. The nurse should advise the client to monitor for signs of bleeding, such as bruising, nosebleeds, or hematuria, and report them to the provider.
Choice B reason: Decreased alertness is not a likely adverse effect of taking gingko biloba, as it may have the opposite effect of enhancing cognitive function and memory. Gingko biloba may improve blood flow to the brain and protect against oxidative stress and neuronal damage. The nurse should inform the client that gingko biloba may take several weeks to show its benefits and that the evidence for its effectiveness is inconclusive.
Choice C reason: Breast enlargement is not a known adverse effect of taking gingko biloba, as it does not affect the hormonal levels or the breast tissue. Gingko biloba may have some estrogenic activity, but it is not significant enough to cause gynecomastia or breast tenderness. The nurse should assess the client for other possible causes of breast enlargement, such as medications, liver disease, or tumors.
Choice D reason: Bad breath is not a common adverse effect of taking gingko biloba, as it does not affect the oral hygiene or the digestive system. Gingko biloba may have a mild odor, but it is not unpleasant or persistent. The nurse should advise the client to maintain good oral care and to check for other possible causes of bad breath, such as infections, dental problems, or dietary factors.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
