A nurse is looking after a patient who is 12 hours postoperative following a transurethral resection of the prostate (TURP) and has a 3-way urinary catheter with continuous irrigation.
The nurse observes that there has been no urinary output in the last hour. What should the nurse do first?
Administer a prescribed analgesic.
Check the patency of the tubing.
Notify the provider.
Offer oral fluids.
The Correct Answer is B
Choice B rationale:
Checking the patency of the tubing is the first and most crucial step in addressing the lack of urinary output in this patient. Here's a detailed explanation of why this is the priority action:
Addresses the Most Likely Cause: Obstruction of the urinary catheter tubing is the most common and easily reversible cause of sudden cessation of urinary output in a patient with a continuous bladder irrigation system.
Prevents Complications: A blocked catheter can lead to a number of serious complications, including: Bladder distention, which can cause pain, discomfort, and potential bladder damage.
Urinary retention, which can increase the risk of urinary tract infections (UTIs) and kidney damage. Hematuria, or blood in the urine, due to clot formation in the bladder or catheter.
Non-Invasive Intervention: Checking the tubing is a simple, non-invasive procedure that can quickly identify and resolve the issue without requiring further interventions or delays in care.
Prioritizes Patient Safety: It's essential to promptly address any potential urinary obstruction to prevent the aforementioned complications and ensure patient safety.
Rationale for Other Choices:
Choice A: Administering a prescribed analgesic:
While pain management is important, it does not directly address the lack of urinary output. Pain medication would be appropriate if pain were assessed to be the cause of the decreased output, but it's not the first priority in this situation.
Choice C: Notifying the provider:
Although the provider should be informed of the situation, checking the tubing for patency is a necessary first step to gather more information and potentially resolve the issue quickly without requiring further intervention.
Choice D: Offering oral fluids:
Increasing fluid intake might be helpful in some cases of decreased urinary output, but it's not the priority action in a patient with a continuous bladder irrigation system and a potential catheter obstruction.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A rationale:
The spinal cord plays a crucial role in pain transmission, but it does not initiate the afferent pathways. It receives pain signals from nociceptors and relays them to the brain for processing.
The spinal cord is also involved in pain modulation, as it can dampen or amplify pain signals depending on various factors. However, it is not the primary trigger for pain sensation. That role belongs to nociceptors.
Choice B rationale:
Nociceptors are specialized sensory receptors that detect potentially damaging stimuli, such as intense heat, pressure, or chemical irritants.
They are located throughout the body, including the skin, muscles, joints, and internal organs.
When nociceptors are activated, they generate electrical signals that travel along nerve fibers to the spinal cord and brain. This process initiates the afferent pathways, which ultimately lead to the conscious perception of pain.
Nociceptors are essential for protecting the body from harm. They alert us to potential dangers and trigger responses that help us avoid injury or further damage.
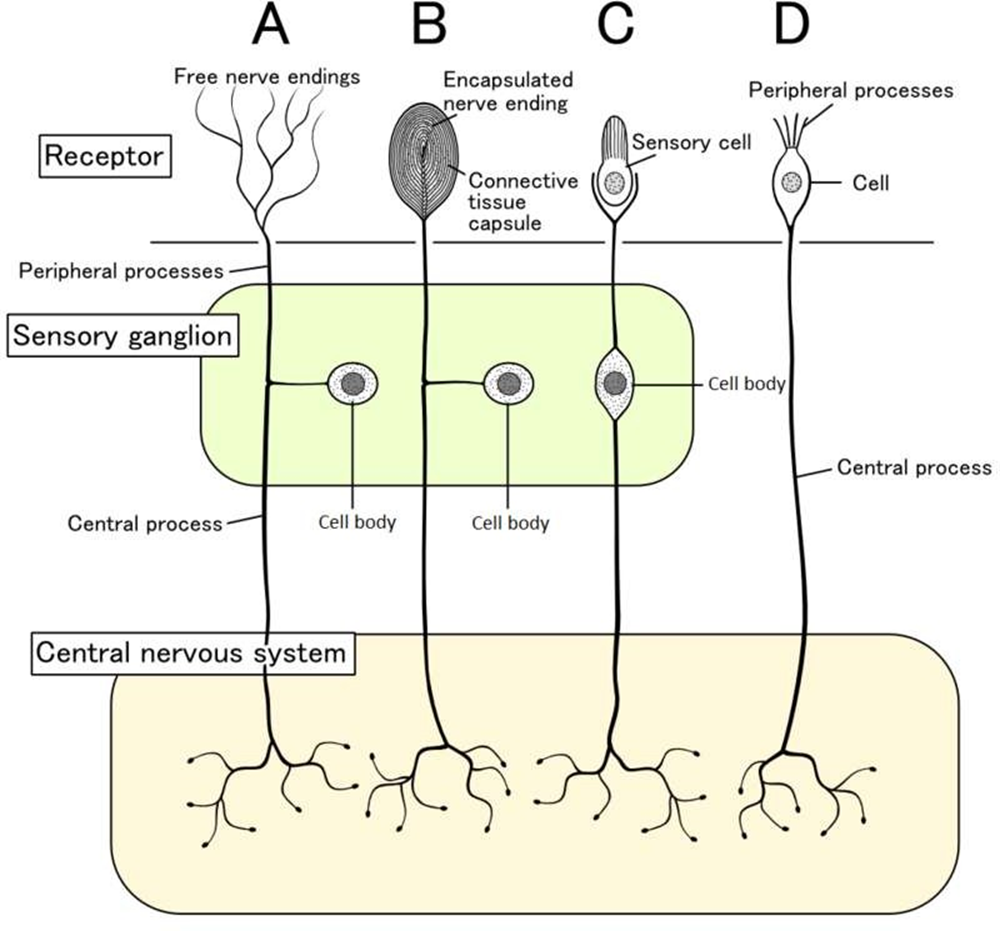
Choice C rationale:
Endorphins are natural pain-relieving substances produced by the body. They act on receptors in the brain and spinal cord to reduce pain perception.
However, endorphins do not trigger the afferent pathways. They work by modulating pain signals that have already been initiated by nociceptors.
Choice D rationale:
The cortex is the outer layer of the brain that is responsible for higher-level functions, such as thinking, feeling, and decision- making.
It plays a role in the conscious experience of pain, but it does not trigger the afferent pathways.
The cortex receives pain signals from the spinal cord and processes them, leading to the awareness of pain.
Correct Answer is D
Explanation
Rationale for Choice A: Obtain vital signs
While obtaining vital signs is important in assessing a patient's overall condition, it is not the first priority in a suspected transfusion reaction.
Vital signs can provide valuable information about the severity of the reaction, but they should not delay the immediate action of stopping the transfusion.
Delaying the cessation of the transfusion could allow for further infusion of incompatible blood or allergens, potentially worsening the reaction and leading to more serious complications.
Rationale for Choice B: Notify the registered nurse
Involving other healthcare professionals is crucial in managing transfusion reactions, but it should not precede stopping the transfusion.
The nurse should prioritize stopping the transfusion to prevent further exposure to potential triggers and then promptly notify the registered nurse for further assessment and interventions.
Timely communication with the registered nurse is essential for coordinating care and ensuring appropriate treatment measures are implemented.
Rationale for Choice C: Administer diphenhydramine
Diphenhydramine, an antihistamine, can be used to treat allergic reactions, but it should not be administered as the first response in this scenario.
The priority is to halt the infusion of the blood product that is potentially causing the reaction.
Administering diphenhydramine before stopping the transfusion could mask the symptoms of the reaction, making it more difficult to assess its severity and progression.
Rationale for Choice D: Stop the transfusion
This is the correct and most immediate action to take when a patient develops itching and hives during a blood transfusion.
These symptoms are indicative of a possible allergic or transfusion reaction, and stopping the transfusion is essential to prevent further complications.
It's critical to act quickly to minimize the amount of incompatible blood or allergens that enter the patient's circulation.
By stopping the transfusion, the nurse can potentially prevent the reaction from worsening and safeguard the patient's well- being.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
