A nurse is caring for a patient on the third day following abdominal surgery.
The nurse notes the absence of bowel sounds, abdominal distention, and the patient has not passed any flatus. Which postoperative complication is the patient likely experiencing?
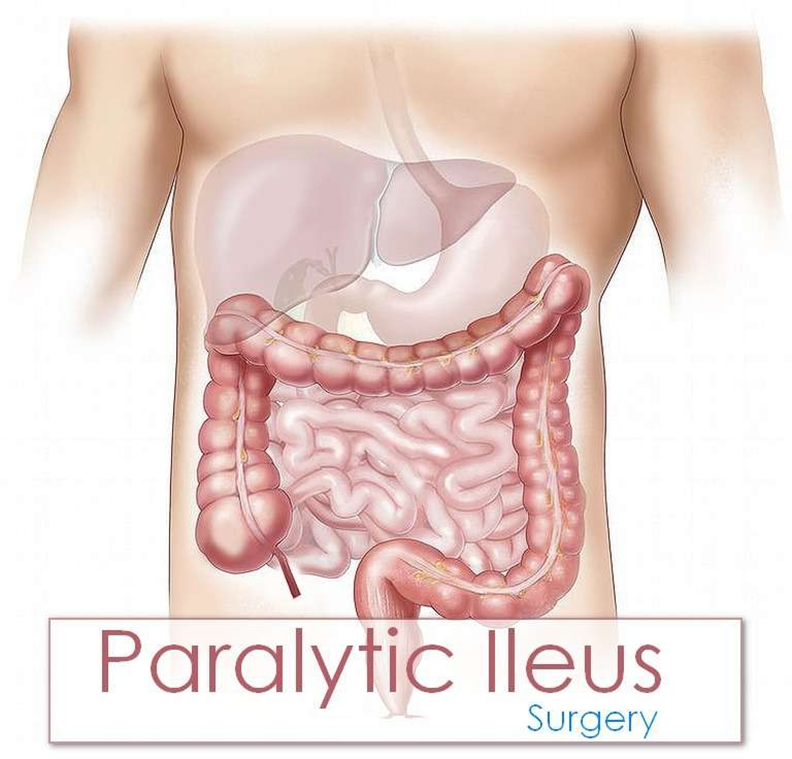
Paralytic ileus
Incisional infection
Fecal impaction
Health care-associated Clostridium difficile
The Correct Answer is A
Choice A rationale:
Paralytic ileus is a common postoperative complication that occurs when the normal movement of the intestines (peristalsis) is slowed or stopped. This can lead to a buildup of gas and fluids in the intestines, causing abdominal distention, nausea, vomiting, and constipation. The absence of bowel sounds, abdominal distention, and the inability to pass flatus are all classic signs of paralytic ileus.
Here are some of the factors that can contribute to paralytic ileus: Manipulation of the intestines during surgery
Anesthesia
Pain medications, especially opioids Electrolyte imbalances
Dehydration
Underlying medical conditions, such as diabetes or kidney disease Treatment for paralytic ileus typically involves:
Resting the bowel by not eating or drinking anything by mouth
Using a nasogastric (NG) tube to suction out gas and fluids from the stomach Providing intravenous (IV) fluids and electrolytes
Encouraging early ambulation
Using medications to stimulate bowel movement, such as metoclopramide or erythromycin
Choice B rationale:
Incisional infection is an infection of the surgical wound. It would typically present with redness, warmth, swelling, and pain at the incision site. The patient may also have a fever. While incisional infections can occur after abdominal surgery, they are not typically associated with the absence of bowel sounds, abdominal distention, and the inability to pass flatus.
Choice C rationale:
Fecal impaction is a severe form of constipation in which a large, hard mass of stool becomes trapped in the rectum. It can cause abdominal pain, bloating, and difficulty passing stool. However, it is not typically associated with the absence of bowel sounds or abdominal distention.
Choice D rationale:
Health care-associated Clostridium difficile (C. difficile) is a bacterial infection that can cause severe diarrhea, abdominal pain, and cramping. It is often associated with antibiotic use. While C. difficile can occur after abdominal surgery, it is not typically associated with the absence of bowel sounds, abdominal distention, and the inability to pass flatus.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A rationale:
It is not necessary to remind a patient to avoid turning from side to side after femoral artery catheterization. Restricting movement in this way could actually increase the risk of complications such as deep vein thrombosis (DVT).
Early ambulation is generally encouraged to promote circulation and prevent blood clots.
Patients are typically allowed to turn and reposition themselves as needed for comfort, unless there are specific contraindications.
Choice B rationale:
Keeping the patient in a high-Fowler's position for 6 hours is not a standard recommendation following femoral artery catheterization.
The patient's position should be based on their individual needs and comfort level.
In some cases, a slight elevation of the head of the bed may be helpful to promote venous return, but prolonged high-Fowler's positioning is not necessary.
Choice C rationale:
Passive range-of-motion exercises are not typically performed on the affected extremity immediately following femoral artery catheterization.
This is because there is a risk of dislodging the catheter or causing bleeding at the puncture site.
Once the catheter has been removed and the puncture site has healed, gentle range-of-motion exercises may be recommended to help maintain joint mobility.
Choice D rationale:
Checking pedal pulses every 15 minutes is essential to assess for adequate circulation to the lower extremities following femoral artery catheterization.
This is because there is a risk of complications such as thrombosis or embolism, which can compromise blood flow to the legs and feet.
If the pedal pulses are weak or absent, it could indicate a serious problem that requires immediate intervention.
Correct Answer is C
Explanation
Choice A rationale:
Bilateral flank pain is not a typical sign of an allergic blood transfusion reaction. It can be associated with other conditions, such as kidney problems, musculoskeletal issues, or abdominal aortic aneurysm. While it's important to assess flank pain, it doesn't directly suggest an allergic reaction to the transfusion.
Choice B Rationale:
Distended jugular veins can indicate fluid overload, which could potentially occur during a transfusion. However, it's not a specific sign of an allergic reaction. Fluid overload can result from various causes, including heart failure, kidney problems, or excessive fluid intake. It's crucial to monitor for fluid overload during transfusions, but it doesn't definitively point to an allergic reaction.
Choice C Rationale:
Generalized urticaria, or hives, is a hallmark sign of an allergic reaction. It's characterized by raised, red, itchy welts that can appear on various parts of the body. Hives can develop rapidly and spread extensively. During a blood transfusion, generalized urticaria strongly suggests that the patient's immune system is reacting to a component of the transfused blood, such as proteins or antibodies.

Choice D Rationale:
Blood pressure 184/92 mm Hg is elevated and could be concerning, but it's not specific to allergic reactions. High blood pressure can have various causes, including stress, pain, anxiety, or underlying hypertension. While monitoring blood pressure during transfusions is essential, it doesn't directly indicate an allergic reaction.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
