A nurse is collecting data from a client who is at 20 weeks of gestation and has been taking ferrous sulfate. For which of the following findings should the nurse monitor as a common adverse effect of iron supplementation and report to the provider?
Dry mouth
Tinnitus
Constipation
Hematuria
The Correct Answer is C
Iron supplementation commonly causes constipation, which is due to the iron's effect of slowing down bowel movements and increasing water absorption in the intestines.
Dry mouth is not a common adverse effect of iron supplementation. It is more commonly associated with medications that can cause xerostomia (dry mouth), such as certain antihistamines or anticholinergic drugs.
Tinnitus, a perception of ringing or noise in the ears, is not typically associated with iron supplementation. Tinnitus can be caused by various factors, such as exposure to loud noises, ear infections, or certain medications, but it is not directly related to iron supplementation.
Hematuria, the presence of blood in the urine, is not a common adverse effect of iron supplementation. It can be caused by various conditions affecting the urinary system, such as urinary tract infections, kidney stones, or bladder issues, but it is not directly related to iron supplementation.

Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
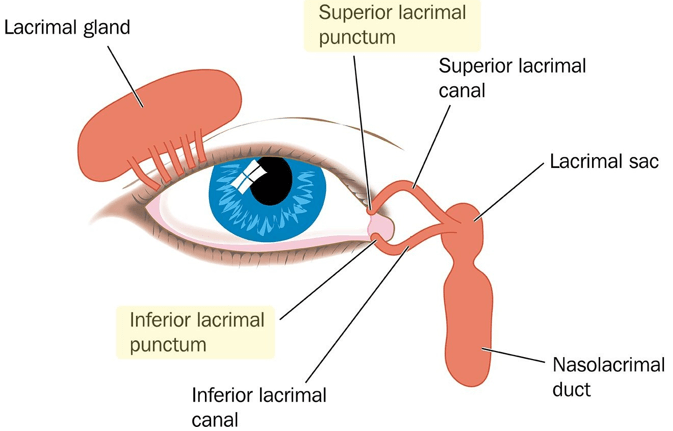
a. Apply pressure to the lacrimal punctum after administering the drops.
When administering eye drops to a child, the nurse should apply gentle pressure to the lacrimal punctum (the small opening in the inner corner of the eye) after administering the drops. This can help prevent the medication from draining into the tear duct and being absorbed into the bloodstream, which can reduce systemic side effects.
Correct Answer is D
Explanation
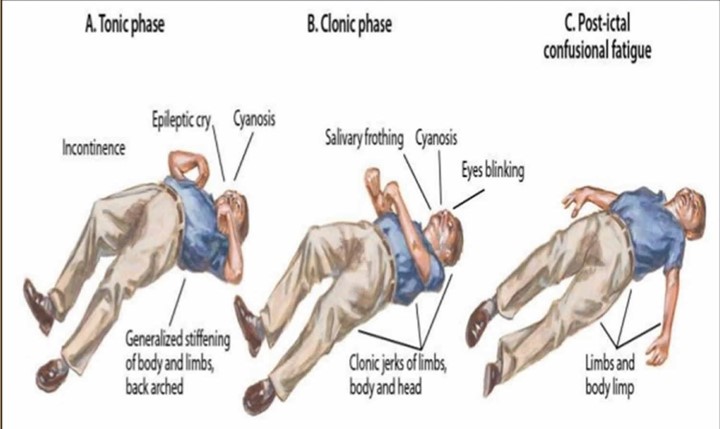
After a tonic-clonic seizure, the nurse should first check the child for any injuries, particularly in the oral cavity. This is because during a seizure, the child's tongue may have been biten, or there may be other oral injuries. Therefore, it is essential to check the oral cavity for any injury or bleeding.
Offering sips of clear fluids is not a priority at this time as the child may still be disoriented and at risk of choking. Placing the child in a supine position is also not recommended because the child may have difficulty breathing due to muscle weakness or constriction of the airways. Administering an oral antiepileptic medication is not appropriate at this time unless prescribed by a healthcare provider.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
