A nurse is collecting data from a client who is 24 hr postpartum. Which of the following findings should the nurse expect?
Fundus soft, 2 fingerbreadths below the umbilicus
Fundus firm, 1 fingerbreadth below the umbilicus
Fundus firm, 4 fingerbreadths above the umbilicus
Fundus soft, to the right of the umbilicus
The Correct Answer is B
Choice A reason: Fundus soft, 2 fingerbreadths below the umbilicus is incorrect, as this finding indicates uterine atony and subinvolution. The fundus is the upper part of the uterus that can be palpated through the abdomen after birth. The fundus should be firm and midline to indicate adequate uterine contraction and involution. A soft or boggy fundus can increase the risk of hemorrhage and infection.
Choice B reason: Fundus firm, 1 fingerbreadth below the umbilicus is correct, as this finding indicates normal uterine contraction and involution. The fundus is normally at the level of the umbilicus immediately after birth and then descends about one fingerbreadth per day. A firm and midline fundus can prevent excessive bleeding and promote healing.
Choice C reason: Fundus firm, 4 fingerbreadths above the umbilicus is incorrect, as this finding indicates a higher than expected fundal height for a client who is 24 hr postpartum. The fundus is normally at the level of the umbilicus immediately after birth and then descends about one fingerbreadth per day. A high fundal height can indicate uterine atony, retained placental fragments, or bladder distension.
Choice D reason: Fundus soft, to the right of the umbilicus is incorrect, as this finding indicates uterine atony and bladder distension. The fundus should be firm and midline to indicate adequate uterine contraction and involution. A deviated fundus can indicate bladder distension, which can interfere with uterine contraction and involution and increase the risk of hemorrhage and infection.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A reason: Fundal consistency is correct, as this finding can indicate the effectiveness of oxytocin in stimulating uterine contraction and preventing postpartum hemorrhage. Oxytocin is a uterotonic agent that can enhance or augment uterine contractility and involution. The nurse should monitor the fundal height, consistency, and position and report any signs of uterine atony or excessive bleeding.
Choice B reason: Fetal heart rate is incorrect, as this finding is not relevant for a client who has already delivered the baby. Fetal heart rate can indicate the fetal well-being and response to labor, but it is not affected by oxytocin administration after birth. The nurse should monitor the newborn's vital signs and appearance and report any signs of distress or infection.
Choice c reason: Urinary output is incorrect, as this finding is not specific for evaluating the effectiveness of oxytocin. Urinary output can indicate the client's renal function and fluid balance, but it can be influenced by many other factors, such as fluid intake, bladder distension, or epidural anesthesia. The nurse should monitor the client's intake and output and report any signs of oliguria or retention.
Choice D reason: Blood pressure is incorrect, as this finding is not specific for evaluating the effectiveness of oxytocin. Blood pressure can indicate the client's hemodynamic status and response to blood loss, but it can be influenced by many other factors, such as pain, anxiety, preeclampsia, or medication. The nurse should monitor the client's vital signs and fluid balance and report any signs of hypotension or hypertension
Correct Answer is A
Explanation
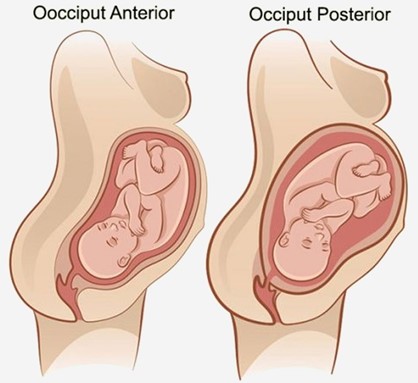
Choice A reason:
Fetal position is persistent occiput posterior is correct, as this position can cause difficult, prolonged labor and severe backache. The occiput posterior position means that the back of the fetal head is facing the maternal sacrum, which can result in poor alignment and descent, increased pressure on the maternal sacrum and nerves, and increased risk of perineal trauma. The nurse should encourage the client to change positions frequently, use pelvic rocking exercises, apply counterpressure to the sacrum, and administer analgesics as needed.
Choice B reason:
Fetal attitude is in general flexion is incorrect, as this attitude can facilitate normal labor and delivery. The fetal attitude refers to the degree of flexion or extension of the fetal head and limbs in relation to the fetal trunk. General flexion means that the fetal head is flexed on the chest, the arms are crossed over the chest, and the legs are flexed at the knees. This attitude allows the smallest diameter of the fetal head to pass through the birth canal.
Choice C reason:
Fetal lie is longitudinal is incorrect, as this lie can facilitate normal labor and delivery. The fetal lie refers to the relationship between the long axis of the fetus and the long axis of the mother. Longitudinal lie means that both axes are parallel, which allows for either a vertex (head-first) or a breech (butocks-first) presentation.
Choice D reason:
Maternal pelvis is gynecoid is incorrect, as this pelvis can facilitate normal labor and delivery. The maternal pelvis refers to the shape and size of the bony pelvis that affects the passage of the fetus. Gynecoid pelvis is the most common and favorable type for vaginal birth, as it has a rounded inlet, a wide pubic arch, and adequate outlet dimensions.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
