A nurse is collecting data from a client who is 12 hr postpartum. Which of the following findings should the nurse expect?
Fundus soft, 2 fingerbreadths below the umbilicus.
Fundus firm, 2 fingerbreadths above the umbilicus.
Fundus soft, to the right of the umbilicus.
Fundus firm, at the level of the umbilicus.
The Correct Answer is D
Choice A reason:
A soft fundus indicates uterine atony, which is a lack of muscle tone that can lead to postpartum hemorrhage. A soft fundus is an abnormal finding and should be reported to the provider. The fundus should be firm and contracted to prevent bleeding.
Choice B reason:
A fundus that is 2 fingerbreadths above the umbilicus is too high for a client who is 12 hours postpartum. The fundus should descend about 1 centimeter per hour after delivery and should be at the level of the umbilicus at 12 hours postpartum. A high fundus could indicate retained placental fragments or a full bladder, both of which can interfere with uterine contraction and cause bleeding.
Choice C reason:
A fundus that is deviated to the right of the umbilicus is also an abnormal finding for a client who is 12 hours postpartum. A deviated fundus could indicate a full bladder, which can displace the uterus and prevent it from contracting properly. The fundus should be at the midline of the abdomen.
Choice D reason:
A fundus that is firm and at the level of the umbilicus is a normal finding for a client who is 12 hours postpartum. This indicates that the uterus is involuting (returning to its pre-pregnancy size and shape) and that there is no excessive bleeding. The nurse should expect this finding and document it accordingly.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["A","B","E"]
Explanation
Choice A:
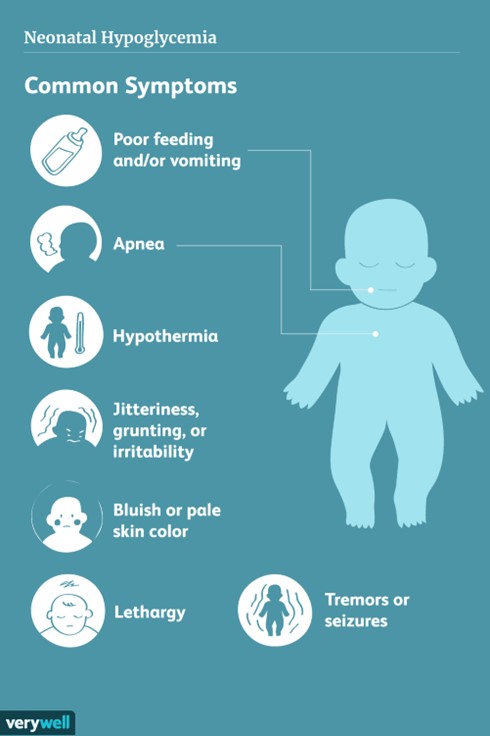
Tremors. This is a sign of hypoglycemia in a newborn because low blood sugar can cause shakiness or jitteriness in the muscles. •
Choice B:
Lethargy. This is a sign of hypoglycemia in a newborn because low blood sugar can cause low energy, poor feeding, or lack of interest in eating.
Choice C:
Hunger. This is not a sign of hypoglycemia in a newborn because low blood sugar can actually reduce the appetite or cause feeding difficulties.
Choice D:
Jaundice. This is not a sign of hypoglycemia in a newborn because jaundice is caused by high levels of bilirubin in the blood, not low levels of glucose.
Choice E:
Weak cry. This is a sign of hypoglycemia in a newborn because low blood sugar can affect the vocal cords and the respiratory system, causing a weak or high-pitched cry.
Correct Answer is B
Explanation
Choice A reason:
Allowing opportunities for newborn massage is not recommended for preterm newborns, as it can increase their oxygen consumption and energy expenditure. Massage can also cause stress responses, such as increased heart rate, blood pressure, and cortisol levels.
Choice B reason:
Clustering the newborn's care activities is the best way to help the newborn conserve energy, as it minimizes the frequency of handling and stimulation. Clustering care also allows for longer periods of uninterrupted sleep, which is essential for growth and development.
Choice C reason:
Changing the newborn's position every 2 hours is not necessary for preterm newborns, as it can disrupt their sleep and cause them to lose heat. Preterm newborns have limited ability to regulate their body temperature, and frequent position changes can expose them to cold stress.
Choice D reason:
Placing elbow restraints on the newborn is not indicated for preterm newborns, unless they have a specific condition that requires them, such as a cleft lip or palate repair. Elbow restraints can restrict the newborn's movement and cause skin irritation or injury.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
