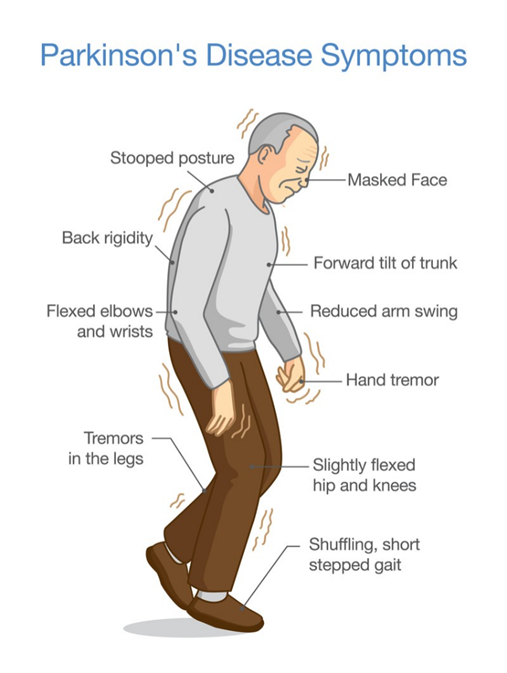
A nurse is collecting data from a client who has Parkinson's disease and is experiencing bradykinesia. Which of the following findings should the nurse expect?
Increased blinking
States of euphoria
Slurred speech
Decreased respiratory rate
The Correct Answer is C
A. Increased blinking
Increased blinking is not a typical manifestation of bradykinesia. In fact, individuals with Parkinson's disease may experience reduced blinking (hypokinesia of blinking) rather than increased blinking.
B. States of euphoria
Euphoria is not typically associated with bradykinesia. Instead, individuals with Parkinson's disease may experience a range of mood changes, including depression, anxiety, or apathy, but euphoria is not a common finding.
C. Slurred speech
This is the correct answer. Slurred speech, or dysarthria, can occur in individuals with Parkinson's disease as a result of bradykinesia affecting the muscles involved in speech production. Bradykinesia can cause a reduction in the speed and coordination of movements necessary for clear speech, resulting in slurred or mumbled speech patterns.
D. Decreased respiratory rate
Decreased respiratory rate is not typically associated with bradykinesia. Bradykinesia primarily affects voluntary movements rather than involuntary processes such as respiration. While respiratory muscle weakness can occur in advanced stages of Parkinson's disease, it is not directly related to bradykinesia.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
A. Insert a padded tongue blade into the client's mouth.
This intervention is not recommended. Placing any object, including a padded tongue blade, into the mouth of someone experiencing a seizure poses a risk of injury, such as biting the tongue or breaking teeth. It can also obstruct the airway and increase the risk of aspiration. Therefore, inserting anything into the client's mouth during a seizure is contraindicated.
B. Place a pillow under the client's head.
Placing a pillow under the client's head can help prevent head injury by providing cushioning and support. It can also help maintain the client's airway and reduce the risk of aspiration. Therefore, this intervention is appropriate and helps ensure the client's safety during the seizure.
C. Gently restrain the client's extremities.
Restraining the client's extremities is not recommended during a seizure. It can increase the risk of injury, such as fractures or dislocations, and may exacerbate muscle contractions. It's important to allow the client's movements to occur naturally while taking measures to ensure their safety, such as removing nearby objects and providing a safe environment.
D. Keep the client in a supine position.
It is essential to ensure that the client's head is turned to the side (recovery position) to prevent aspiration and allow for drainage of oral secretions. Additionally, the nurse should remove any nearby objects that could pose a risk of injury during the seizure.
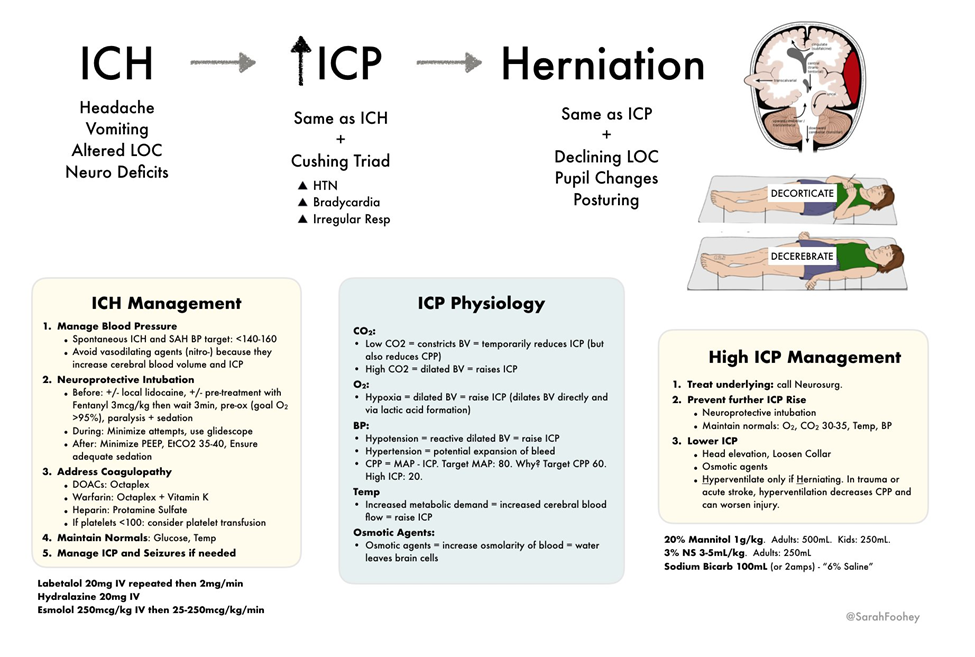
Correct Answer is C
Explanation
A. Instruct the client to perform controlled coughing and deep breathing.
This intervention is not appropriate for a client with increased intracranial pressure. Controlled coughing and deep breathing can increase intrathoracic pressure, which can in turn increase intracranial pressure. Therefore, this intervention should be avoided in clients with increased ICP.
B. Provide a brightly lit environment.
This intervention is not appropriate for a client with increased intracranial pressure. Bright lights can stimulate the reticular activating system and increase arousal, potentially exacerbating cerebral metabolic demand and intracranial pressure. Therefore, it is recommended to provide a calm, quiet environment with subdued lighting for clients with increased ICP.
C. Elevate the head of the bed 30°.
This intervention is correct. Elevating the head of the bed to 30 degrees promotes venous drainage from the head and reduces intracranial pressure. It helps prevent venous congestion in the brain and improves cerebral perfusion. This position is commonly used in clients with increased intracranial pressure to optimize cerebral blood flow.
D. Encourage a minimum intake of 2,000 mL/day of clear fluids.
This intervention is not appropriate for a client with increased intracranial pressure. While maintaining hydration is important for overall health, excessive fluid intake can increase intracranial pressure by increasing cerebral blood volume and cerebrospinal fluid production. Therefore, fluid intake should be carefully monitored and adjusted based on the client's condition and fluid balance.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
