A nurse is caring for a newly admitted older adult client.
Nurses' Notes
Day 1, 12:00:
Transferred to the medical-surgical unit from the emergency department (ED) for continued care following a closed reduction and immobilization of a fracture of the right arm. Accompanied by an adult child.
Client in visibly soiled night clothes with multiple stains, including what appears to be dried blood. Hair, teeth, and fingernails unclean. Strong body odor noted. Bruising of various stages noted around upper arms, back, shoulders, and neck area.
The client is soft-spoken, speaks almost in a whisper, and does not make eye contact with the nurse.
The client looks at their child before answering the nurse's questions and, when asked how the injury occurred, mumbles "I don't know. Ask them." The client's child states, "He gets confused sometimes. I can answer your questions."
Which of the following interventions should the nurse recommend to include in the client's plan of care?
Select all that apply.
Tell the client's child that they will be reported for maltreatment of the client.
Ask the client's child to provide details regarding the client's fractured arm.
Discuss respite care options with the client's child.
Speak to the client privately.
Provide legal advice to the client regarding the power of attorney.
Correct Answer : B,C,D
It is not appropriate for the nurse to threaten the client's child with reporting for maltreatment without further assessment and evidence.
Asking the client's child to provide details regarding the client's fractured arm will provide additional information about the client's injury and help the nurse assess the potential for abuse or neglect.
Discussing respite care options with the client's child may help alleviate any caregiver stress or burden, and ensure the client's continued care and safety.
Speaking to the client privately will help establish trust and rapport, and allow the client to disclose any
concerns or issues that they may not feel comfortable sharing in front of their child.
Providing legal advice regarding power of attorney is not within the scope of nursing practice and should be referred to a legal professional. Additionally, the client's capacity to make decisions and appoint a power of attorney should be assessed before providing such advice.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
The nurse should identify that disposing of contaminated sheets in a linen bag demonstrates effective use of supplies.
Wearing an N95 mask when bathing a client with Clostridium difficile is important, but it is not related to effective use of supplies.
Wearing clean gloves when performing oral hygiene is standard practice for infection control and not specific to the use of supplies.
Empting the sharps container when it is full is also important, but it is not related to effective use of supplies.
Correct Answer is A
Explanation
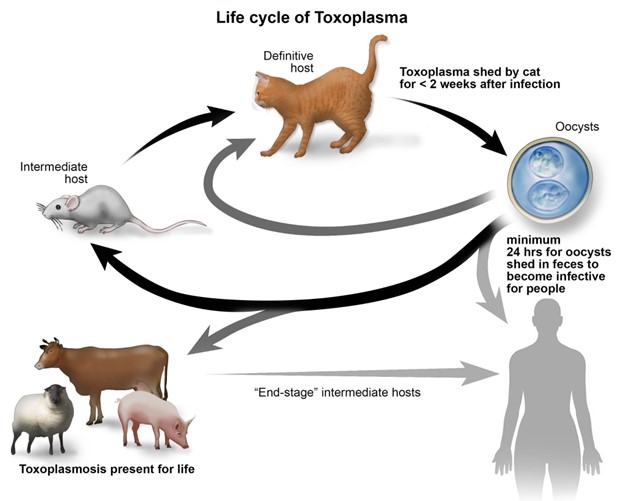
Toxoplasmosis is an infection caused by the Toxoplasma gondii parasite. The primary mode of transmission is through the ingestion of the parasite's oocysts, which are commonly found in cat feces.
When a person comes into contact with cat feces, such as during cleaning of the litter box or gardening in soil contaminated with cat feces, they can inadvertently ingest the parasite. Therefore, handling cat feces is a common route of transmission for toxoplasmosis.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
