A nurse is caring for a client who is in labor. Which of the following findings should prompt the nurse to reassess the client?
An urge to have a bowel movement during contractions
A sense of excitement and warm, flushed skin
Progressive sacral discomfort during contractions
Intense contractions lasting 45 to 60 seconds
The Correct Answer is A
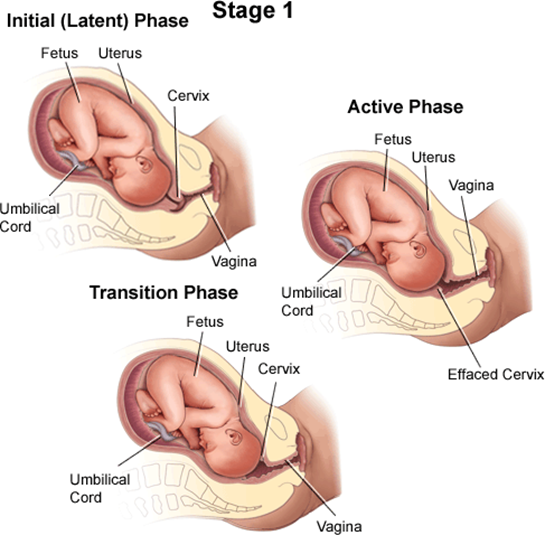
A client who is in labor and reports an urge to have a bowel movement during contractions may be experiencing the transition phase of labor, which is the last and most intense part of the first stage of labor¹². The transition phase occurs when the cervix dilates from 8 to 10 cm and the baby descends into the birth canal¹². The pressure of the baby's head on the rectum can cause a sensation of needing to defecate¹². The transition phase can last from 15 minutes to an hour or more, and it can be accompanied by other signs, such as strong, regular, and painful contractions lasting 60 to 90 seconds; increased bloody show; nausea and vomiting; shaking and shivering; and emotional changes such as irritability, anxiety, or excitement¹²³.
The nurse should reassess the client who reports an urge to have a bowel movement during contractions because this may indicate that the client is close to delivering the baby and needs to be prepared for the second stage of labor, which involves pushing and giving birth¹². The nurse should check the client's cervical dilation, fetal heart rate, and maternal vital signs, and notify the provider if the client is fully dilated or shows signs of fetal or maternal distress¹². The nurse should also support the client's coping strategies, such as breathing techniques, relaxation methods, or pain relief options, and encourage the client not to push until instructed by the provider¹².
b) A sense of excitement and warm, flushed skin are not signs that require reassessment by the nurse. These are normal emotional and physiological responses to labor that reflect increased adrenaline levels and blood flow¹⁴. They do not indicate any complications or imminent delivery.
c) Progressive sacral discomfort during contractions is not a sign that requires reassessment by the nurse. This is a common symptom of labor that results from the pressure of the baby's head on the sacrum and nerves in the lower back¹⁴. It does not indicate any problems or imminent delivery.
d) Intense contractions lasting 45 to 60 seconds are not signs that require reassessment by the nurse. These are typical characteristics of active labor contractions, which occur when the cervix dilates from 4 to 8 cm¹⁴. They do not indicate any complications or imminent delivery.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Late decelerations are a type of fetal heart rate (FHR) pattern that indicate fetal hypoxia (lack of oxygen) due to uteroplacental insufficiency (decreased blood flow to the placenta). They are defined as a gradual decrease in FHR that occurs after the peak of a uterine contraction and returns to baseline after the end of the contraction¹. Late decelerations are associated with adverse neonatal outcomes, such as low Apgar scores, acidosis, and neonatal intensive care unit admission².
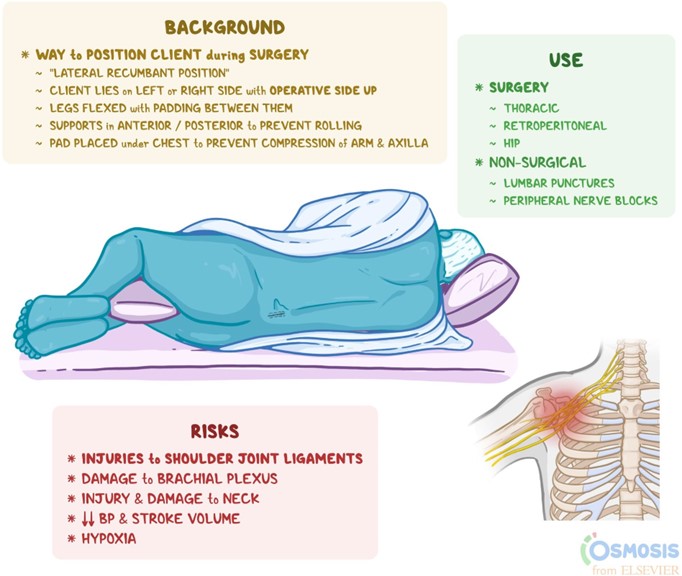
The nurse should take immediate actions to improve fetal oxygenation and blood flow when late decelerations are detected. The first and most important action is to place the client in a lateral position, either left or right, to reduce compression of the inferior vena cava and increase uterine perfusion. This can improve fetal oxygenation and reduce the severity of late decelerations¹³.
The other actions that the nurse should take are:
- Discontinue oxytocin infusion if it is being used for induction or augmentation of labor, as it can cause uterine tachysystole (excessive contractions) and worsen uteroplacental insufficiency¹³.
- Administer oxygen to the client at 8 to 10 L/min via a nonrebreather face mask to increase maternal oxygen saturation and fetal oxygen delivery¹³.
- Increase intravenous (IV) fluid infusion rate to maintain maternal hydration and blood pressure, which can improve uterine blood flow¹³.
- Notify the provider and prepare for possible operative delivery if late decelerations persist or fetal distress occurs¹³.
- Provide emotional support and reassurance to the client and family, as late decelerations can cause anxiety and fear⁴.
The other options are not actions that the nurse should take:
- a) Administer misoprostol 25 mcg vaginally. This is not correct because misoprostol is a medication that is used to induce labor by ripening the cervix and stimulating contractions. It is not indicated for late decelerations and can cause uterine hyperstimulation and fetal distress⁵.
- c) Administer oxygen via a face mask at 2 L/min. This is not correct because this is too low of an oxygen flow rate to improve fetal oxygenation. The recommended oxygen flow rate for late decelerations is 8 to 10 L/min via a nonrebreather face mask¹³.
- d) Decrease the maintenance IV solution infusion rate. This is not correct because this can cause maternal dehydration and hypotension, which can reduce uterine blood flow and worsen fetal hypoxia. The nurse should increase the IV fluid infusion rate to maintain maternal hydration and blood pressure¹³.
Correct Answer is B
Explanation
Among the given options, the client who is at 34 weeks of gestation and experiencing epigastric pain and headache should be assessed first. Epigastric pain and headache can be signs of preeclampsia, a serious condition characterized by high blood pressure and organ dysfunction during pregnancy. Preeclampsia requires immediate attention as it can lead to complications for both the mother and the fetus.
Option a) A client at 12 weeks of gestation experiencing nausea and vomiting may be experiencing normal symptoms of early pregnancy. While it is important to assess the client's well-being, it is not an immediate priority compared to the potential signs of preeclampsia in option b.
Option c) A client at 38 weeks of gestation experiencing painful urination may indicate a urinary tract infection (UTI). While a UTI should be addressed, it does not pose the same level of immediate risk as the potential signs of preeclampsia in option b.
Option d) A client at 39 weeks of gestation experiencing cramping and spotting may be in early labor or have other signs of impending labor. While it is important to assess this client's condition, it is not an immediate priority compared to the potential signs of preeclampsia in option b.
Therefore, the nurse should assess the client who is at 34 weeks of gestation and experiencing epigastric pain and headache as the first priority. Prompt evaluation and management of preeclampsia symptoms are crucial to prevent complications and ensure the well-being of both the mother and the fetus.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
