A nurse is caring for a client who is immobile.
Which of the following interventions is appropriate to prevent contracture?
Align a trochanter wedge between the client’s legs.
Apply an orthotic to the client’s foot.
Place a towel roll under the client’s neck.
Position a pillow under the client’s knees.
undefined
The Correct Answer is B
The correct answer is choice B. Applying an orthotic to the client’s foot.
An orthotic is a device that supports or corrects the function of a body part.
In this case, an orthotic can help prevent foot drop, which is a common contracture deformity in immobile patients.
Foot drop occurs when the muscles that lift the foot become weak or paralyzed, causing the foot to hang down at the ankle. An orthotic can keep the foot in a neutral position and prevent shortening of the calf muscles and Achilles tendon.
Choice A is wrong because a trochanter wedge is used to prevent external rotation of the hip, not contracture. A trochanter wedge is a triangular-shaped pillow that is placed between the legs to keep them parallel and aligned.
Choice C is wrong because a towel roll under the neck is used to maintain proper cervical alignment, not contracture. A towel roll can prevent hyperextension of the neck and support the natural curve of the spine.
Choice D is wrong because a pillow under the knees can actually cause contracture of the knee joint by keeping it in a flexed position. A pillow under the knees can also reduce blood flow to the lower extremities and increase the risk of deep vein thrombosis.
Contracture is a permanent tightening of the muscles, tendons, skin, and surrounding tissues that causes the joints to shorten and stiffen.
Contracture can limit the range of motion and function of the affected body part. Contracture can be caused by inactivity, scarring, or diseases that affect the muscles or nerves. Prevention of contractures requires early diagnosis and initiation of physical medicine approaches such as passive range of motion exercises and splinting before contractures are present or while contractures are mild.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
This is a sign of preeclampsia, a serious complication of pregnancy that can cause high blood pressure, proteinuria, and seizures.
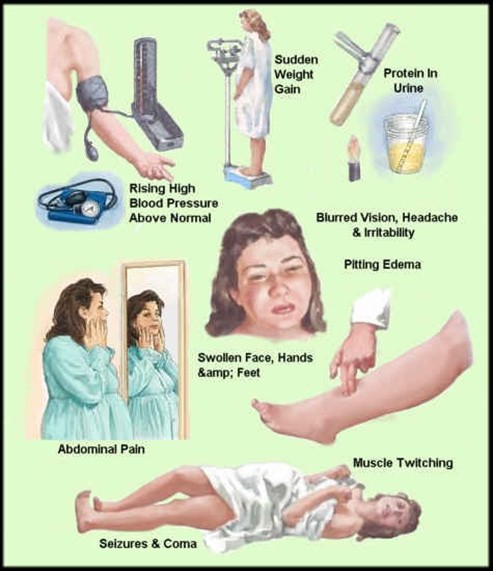
Preeclampsia can affect the placenta, the kidneys, the liver, and the brain of the mother and the fetus. It requires immediate medical attention and may lead to early delivery.
Choice A, bleeding gums, is wrong because it is a common occurrence during pregnancy due to hormonal changes that increase blood flow to the gums. It is not a cause for concern unless it is excessive or accompanied by other symptoms.
Choice B, urinary frequency, is wrong because it is also a normal finding during pregnancy due to the growing uterus putting pressure on the bladder. It is not a sign of infection or kidney problems unless it is associated with pain, burning, or blood in the urine.
Choice D, faintness upon rising, is wrong because it is usually caused by orthostatic hypotension, a drop in blood pressure when changing positions.
This can happen during pregnancy due to the dilation of blood vessels and the increased blood volume. It can be prevented by rising slowly, drinking enough fluids, and avoiding prolonged standing.
Correct Answer is C
Explanation
The correct answer is C. Explain to the child what will happen when the abuse is reported.
This is because the nurse should provide honest and accurate information to the child about the reporting process and the possible outcomes, such as legal actions, investigations, or removal from the home.
This can help the child feel more prepared and less anxious about what will happen next. The nurse should also reassure the child that the abuse is not their fault and that they did the right thing by telling someone.
Choice A is wrong because reassuring the child that no one will be told about the abuse is unethical and illegal.
The nurse has a mandatory duty to report any suspected or confirmed cases of child abuse to the appropriate authorities, such as child protective services or law enforcement. Keeping the abuse a secret can also endanger the child’s safety and well-being, as well as prevent them from receiving the necessary medical and psychological care.
Choice B is wrong because ensuring that multiple nurses are present for the physical examination can increase the child’s fear, embarrassment, or discomfort.
The nurse should minimize the number of people involved in the examination and only include those who are essential for providing care or collecting evidence. The nurse should also explain to the child what will be done during the examination and obtain their consent before proceeding.
Choice D is wrong because using leading statements to obtain information from the child can influence their responses and affect the validity of their testimony.
The nurse should use open-ended questions and avoid suggesting or implying any details about the abuse. The nurse should also document the child’s statements verbatim and avoid interpreting or paraphrasing them.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
