A nurse is caring for a client who has bleeding esophageal varices and is being treated with a Sengstaken-Blakemore tube. Which of the following actions should the nurse perform?
Deflate the balloons for 5 min every 2 hr to prevent tissue necrosis.
Keep the head of the bed flat at all times to prevent the development of shock.
Maintain constant observation while the balloons are inflated.
Suction the tube every 2 hr and as needed to maintain patency.
Suction the tube every 2 hr and as needed to maintain patency.
The Correct Answer is C
Choice A Reason: This is incorrect. The balloons should not be deflated without a physician's order, as this can cause rebleeding or aspiration.
Choice B Reason: This is incorrect. The head of the bed should be elevated to 30 to 45 degrees to reduce pressure on the balloons and prevent gastric reflux.
Choice C Reason: This is correct. The nurse should monitor the client closely for signs of complications, such as airway obstruction, aspiration, or balloon rupture. The nurse should also keep scissors at the bedside to cut the tube and release the balloons in case of an emergency.
Choice D Reason: This is incorrect. The tube should not be suctioned, as this can damage the mucosa and cause bleeding. The nurse should only aspirate gastric contents through the gastric lumen to decompress the stomach.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
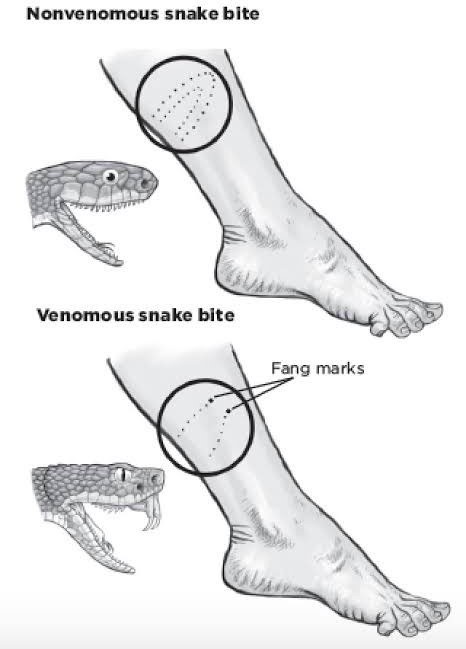
Choice A: Removing the elastic bandages is not recommended. These bandages help slow the spread of venom by compressing the lymphatic vessels. Removing them could worsen the envenomation.
Choice B: This is incorrect. The nurse should not discharge the client, as they may develop serious complications from the snake bite, such as swelling, bleeding, infection, or shock. The client should be monitored closely and treated accordingly.
Choice C: This is the correct action. Antivenom treatment is crucial for serious snake envenomation. The sooner it can be administered, the better the outcome.
Choice D: While pain management is important, it is not the priority in this situation. Antivenom takes precedence over pain medication.
Correct Answer is ["A","B","D","E"]
Explanation
Choice a) is correct because copies of insurance cards can help clients access medical care and claim compensation in case of a disaster. Insurance cards can also serve as a form of identification if other documents are lost or damaged.
Choice b) is correct because a whistle can help clients signal for help or locate each other in case of an emergency. A whistle can also deter potential atackers or wild animals.
Choice c) is incorrect because antibiotics are not recommended to be included in a disaster readiness supply kit or “go bag”. Antibiotics are prescription drugs that should only be used under the guidance of a health care provider. Using antibiotics without proper indication, dosage, or duration can cause adverse effects, such as allergic reactions, resistance, or superinfection.
Choice d) is correct because household bleach can be used to disinfect water, surfaces, or wounds in case of a disaster. Household bleach can also be used to create chlorine gas, which can be used as a weapon or a deterrent.
Choice e) is correct because pencil and paper can be used to write down important information, such as contact numbers, medical history, or evacuation plans. Pencil and paper can also be used to communicate with others, especially if there is no access to phone or internet services.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
