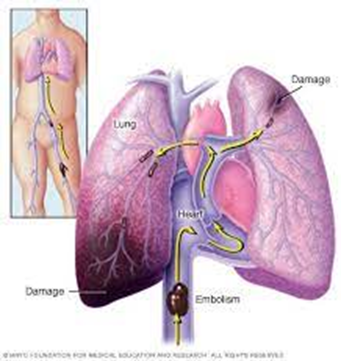
A nurse is caring for a client who has a pulmonary embolism. The nurse should identify that the release of inflammatory mediators leads to which of the following pathologic findings?
Decreased pulmonary vascular resistance
Hypercapnia
Hypoventilation
Respiratory alkalosis
The Correct Answer is D
Correct answer: D
Choice A Reason:
Decreased pulmonary vascular resistance is incorrect. Inflammatory mediators released in response to a pulmonary embolism can lead to vasoconstriction and increased pulmonary vascular resistance. This is part of the body's response to redirect blood flow away from the affected area of the lung and maintain adequate perfusion to other areas.
Choice B Reason:
Hypercapnia is incorrect. Hypercapnia refers to elevated levels of carbon dioxide (CO2) in the blood. Hypocapnia usually is present with embolism; hypercapnia, on the other hand, is rare.
Choice C Reason:
Hypoventilation is incorrect. Hypoventilation occurs when there is inadequate ventilation of the lungs relative to metabolic demands. In the context of a pulmonary embolism, hypoventilation can occur due to factors such as pain, respiratory muscle fatigue, or impaired gas exchange, all of which can be influenced by the release of inflammatory mediators.
Choice D Reason:
Respiratory alkalosis is correct. In response to the blockage and the resulting inflammation, the body often increases the respiratory rate as a compensatory mechanism to maintain adequate oxygen levels and remove carbon dioxide. Due to the increased breathing rate, there is excessive exhalation of carbon dioxide, leading to a decrease in the partial pressure of CO2 in the blood. This results in an increase in blood pH, causing respiratory alkalosis.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A Reason:
The client has no sensation or movement below the level of the injury is correct. This is a characteristic finding of a complete spinal cord injury, where there is total loss of sensory and motor function below the level of the injury. This pattern is often seen in injuries involving the cervical spinal cord, such as at the level of C7.
Choice B Reason:
The client has some movement but no sensation below the level of the injury is incorrect. This finding would be more indicative of an incomplete spinal cord injury, where there is partial preservation of sensory or motor function below the level of the injury. However, with a transection of the spinal cord at C7, it is less likely for the client to have retained movement below the level of injury.
Choice C Reason:
The client has some movement and also some sensation below the level of the injury is incorrect. This finding is not typically associated with a spinal cord injury at the level of C7. With a transection of the spinal cord at this level, there is typically complete loss of sensory and motor function below the level of the injury.
Choice D Reason:
The client has some sensation but no movement below the level of the injury is incorrect. This finding is more consistent with an incomplete spinal cord injury, where there may be partial preservation of sensory function but no motor function below the level of the injury. However, with a transection of the spinal cord at C7, it is less likely for the client to have retained sensation below the level of injury.
Correct Answer is D
Explanation
Choice A Reason:
Dulaglutide is inappropriate. Dulaglutide is a medication used to treat type 2 diabetes by improving blood sugar control. It is not indicated for the management of neurogenic bladder or urinary incontinence.
Choice B Reason:
Montelukast sodium is inappropriate. Montelukast sodium is a medication primarily used to treat asthma and allergic rhinitis by blocking leukotrienes, which are inflammatory substances that contribute to asthma and allergy symptoms. It is not indicated for the management of neurogenic bladder or urinary incontinence.
Choice C Reason:
Glatiramer acetate is inappropriate. Glatiramer acetate is a medication used to treat relapsing-remitting multiple sclerosis (MS) by modulating the immune system. It is not indicated for the management of neurogenic bladder or urinary incontinence.
Choice D Reason:
Oxybutynin is appropriate. Oxybutynin is a medication commonly prescribed for the management of neurogenic bladder and urinary incontinence. It belongs to a class of medications called anticholinergics, which work by relaxing the bladder muscles and reducing bladder spasms. Oxybutynin helps control urinary urgency, frequency, and incontinence associated with neurogenic bladder, including spasm-induced incontinence.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
