A nurse is assisting with the admission of a 9-year-old child who has acute rheumatic fever. When obtaining the client's history, it is appropriate for the nurse to ask the parent which of the following questions?
"Has your son had a sore throat recently?"
"Was your son born with this cardiac defect?"
"Are you aware that your son will have to be in isolation?
"Has your child had any injuries recently?"
The Correct Answer is A
A. "Has your son had a sore throat recently?"
This question is relevant because acute rheumatic fever often occurs as a complication of untreated or inadequately treated streptococcal throat infection (strep throat). A recent history of sore throat could indicate a preceding streptococcal infection, which is an important predisposing factor for the development of acute rheumatic fever.
B. "Was your son born with this cardiac defect?"
This question is less relevant in the context of acute rheumatic fever. Acute rheumatic fever is not a congenital heart defect; it is an inflammatory condition that affects the heart valves following streptococcal infection. While it's important to assess the child's cardiac health, asking about congenital heart defects may not directly relate to the current condition.
C. "Are you aware that your son will have to be in isolation?"
This question is not applicable to acute rheumatic fever. Acute rheumatic fever is not a contagious condition that requires isolation. It is an autoimmune response triggered by streptococcal infection and does not pose a risk of transmission to others.
D. "Has your child had any injuries recently?"
Inquiring about recent injuries is not directly related to acute rheumatic fever. Acute rheumatic fever is an inflammatory condition primarily triggered by streptococcal infection and is not caused by physical injuries.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
A. "Your child's diet should be high in carbohydrates & proteins with no restriction of fats."
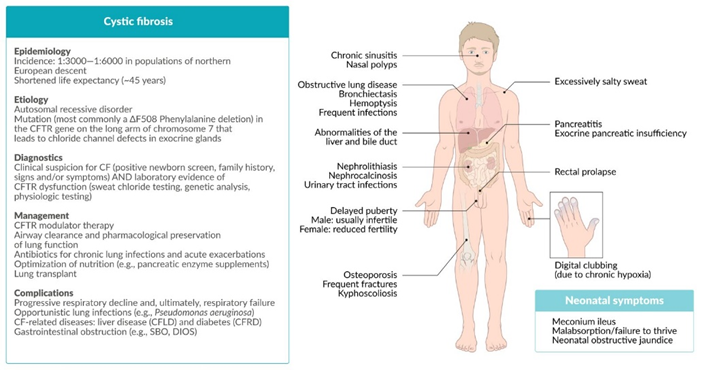
This statement is not entirely accurate. While it's true that children with cystic fibrosis often require a diet that is higher in calories and protein to support growth and weight gain, there is typically a need to restrict fat intake. Pancreatic insufficiency, which is common in cystic fibrosis, can lead to malabsorption of fats and fat-soluble vitamins. Therefore, a dietitian may recommend enzyme replacement therapy and a diet that is moderate in fat but high in calories and protein.
B. "Limit your child's intake of sodium to avoid complications."
This statement is not accurate. Cystic fibrosis can lead to excessive loss of salt in sweat, which can contribute to dehydration and electrolyte imbalances. Therefore, limiting sodium intake can cause electrolyte disturbances.
C. "A pigeon-shaped chest might become evident as the disease progresses."
This statement is accurate. Cystic fibrosis can cause chronic lung infections and inflammation, leading to structural changes in the chest over time. One common manifestation is a barrel-shaped or "pigeon-shaped" chest, which can occur as the disease progresses. This may result from hyperinflation of the lungs due to air trapping and chronic respiratory compromise.
D. "Administer a bronchodilator to the child after chest percussion therapy."
This statement is not necessarily accurate or applicable to all cases. Bronchodilators are medications used to help relax and open the airways in conditions such as asthma or chronic obstructive pulmonary disease (COPD). While bronchodilators may be part of the treatment regimen for some individuals with cystic fibrosis, their use after chest percussion therapy would depend on the individual's specific respiratory symptoms and treatment plan. It's important for the parents to follow the healthcare provider's instructions regarding medication administration.
Correct Answer is A
Explanation
A. Give the child a stuffed animal: Providing a comforting item like a stuffed animal can help the child feel more secure and may offer some comfort during the parent's absence. This option is appropriate as it addresses the child's emotional needs.
B. Inform the child that her parent will be back in 2 hours: While it's helpful to provide reassurance to the child, a 2-year-old may not fully understand the concept of time, and telling them that their parent will return in 2 hours may not effectively alleviate their distress. This option may not be as immediately comforting as providing a tangible source of comfort.
C. Call the parent to return to the child's room: If possible, having the parent return to the child's room can provide the most direct comfort and reassurance to the child during a tantrum. However, it may not always be feasible for the parent to return immediately, especially if they are occupied or attending to other responsibilities.
D. Leave the child alone in the room for 5 minutes: Leaving the child alone during a tantrum can exacerbate feelings of distress and abandonment, potentially escalating the situation further. It's essential to provide support and reassurance to the child during moments of distress rather than leaving them alone.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
