A nurse is caring for a 4-year-old child who is 2 days postoperative following the insertion of a ventriculoperitoneal shunt. Which of the following findings should the nurse identify as the priority?
Lethargy
Urine output 70 mL in 2 hr
Lying flat on the unaffected side
Respiratory rate 20/min
The Correct Answer is A
A. Lethargy: Lethargy can be a concerning sign in a postoperative child, especially following a procedure involving the central nervous system like VP shunt insertion. It could indicate increased intracranial pressure or other neurological complications, which require immediate attention. Therefore, this is a priority finding.
B. Urine output 70 mL in 2 hr: While monitoring urine output is important for assessing hydration and renal function, a urine output of 70 mL in 2 hours may not be immediately concerning in a 4-year-old child. However, if this pattern continues or if there are signs of dehydration, it should be addressed. It's not as urgent as assessing for neurological changes.
C. Lying flat on the unaffected side: The positioning of the child, lying flat on the unaffected side, may or may not be concerning depending on the specific instructions provided postoperatively. While positioning can affect the function of the VP shunt, it may not necessarily indicate an immediate complication.
D. Respiratory rate 20/min: A respiratory rate of 20 breaths per minute is within the normal range for a 4-year-old child. While changes in respiratory rate can indicate respiratory distress, this respiratory rate alone is not immediately concerning.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
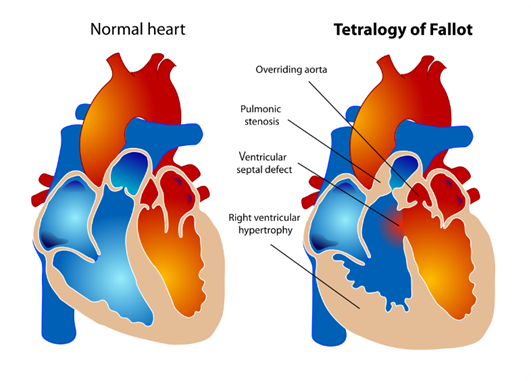
A. Overriding aorta: In Tetralogy of Fallot, the aorta is positioned over the ventricular septal defect (VSD), rather than solely over the left ventricle as it would be in a normal heart. This is called overriding aorta, which allows blood from both the right and left ventricles to enter the aorta.
B. Pulmonary stenosis: This is a critical component of Tetralogy of Fallot. Pulmonary stenosis refers to narrowing of the pulmonary valve or the area just below it, which restricts blood flow from the right ventricle to the pulmonary artery. This results in decreased blood flow to the lungs for oxygenation.
C. Left ventricular hypertrophy: This choice is not typically associated with Tetralogy of Fallot. Left ventricular hypertrophy refers to an enlargement or thickening of the muscular wall of the left ventricle of the heart. It is often seen in conditions where the left ventricle has to work harder to pump blood, such as in hypertension or aortic stenosis, but it is not a characteristic feature of Tetralogy of Fallot.
D. Ventricular septal defect: This defect is one of the four components of Tetralogy of Fallot. A ventricular septal defect (VSD) is a hole in the septum, the muscular wall that separates the left and right ventricles of the heart. In Tetralogy of Fallot, the VSD allows oxygen-poor blood from the right ventricle to flow directly into the left ventricle and out to the body.
Correct Answer is B
Explanation
A. Methylprednisolone: Methylprednisolone is a corticosteroid used for long-term management and prevention of asthma exacerbations. It has anti-inflammatory effects and is not typically used for immediate relief during an acute asthma attack.
B. Albuterol: Albuterol is a short-acting beta-agonist bronchodilator, which is the first-line medication for relieving acute bronchoconstriction during an asthma attack. It works quickly to open the airways and improve breathing.
C. Fluticasone: Fluticasone is an inhaled corticosteroid used for long-term asthma control and prevention of symptoms. It has anti-inflammatory effects but is not used for immediate relief during an acute asthma attack.
D. Beclomethasone: Beclomethasone is also an inhaled corticosteroid used for long-term asthma control and prevention of symptoms. Like fluticasone, it is not used for immediate relief during an acute asthma attack.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
