A nurse is assessing a client who is experiencing an anaphylactic reaction to an antibiotic. Which of the following manifestations of anaphylaxis should the nurse expect?
Hypertonic reflexes
increase in systolic blood pressure
Angioedema
Urinary retention
The Correct Answer is C
The nurse should expect angioedema as one of the manifestations of anaphylaxis in a client experiencing an allergic reaction to an antibiotic. Angioedema is a severe swelling that occurs beneath the skin, typically affecting the face, lips, tongue, throat, or other body parts. It is a result of the release of histamine and other inflammatory mediators in response to the allergen.
Anaphylaxis is a life-threatening allergic reaction that can occur rapidly and affect multiple body systems. In addition to angioedema, other common manifestations of anaphylaxis include:
-
Difficulty breathing or wheezing due to bronchospasm
-
Hives or urticaria, which are itchy raised skin rashes
-
Severe itching or tingling sensation
-
Rapid and weak pulse
-
Low blood pressure leading to hypotension
-
Nausea, vomiting, or diarrhea
-
Feeling of impending doom or anxiety
Let's go through the other options:
A. Hypertonic reflexes: This is not a manifestation of anaphylaxis. "Hypertonic reflexes" are not typically associated with allergic reactions or anaphylaxis. Hypertonic reflexes refer to increased muscle tone, but they are not part of the usual presentation of anaphylaxis.
B. Increase in systolic blood pressure: Anaphylaxis usually leads to a decrease in blood pressure rather than an increase. The decrease in blood pressure can be severe and result in shock, which is a life-threatening condition.
D. Urinary retention: Urinary retention is not a common manifestation of anaphylaxis. Anaphylaxis primarily affects the respiratory and circulatory systems, leading to airway constriction, difficulty breathing, and cardiovascular collapse. Urinary retention is not directly related to the pathophysiology of anaphylaxis.

Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
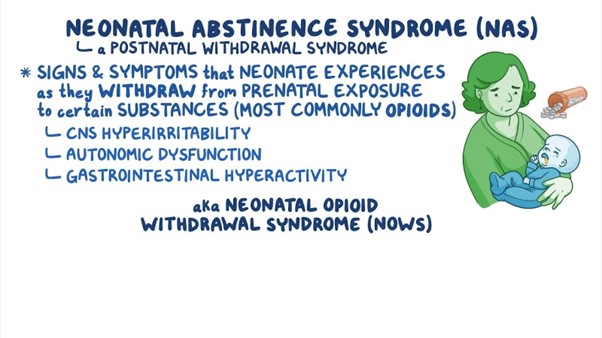
Neonatal abstinence syndrome (NAS) is a group of withdrawal symptoms that occur in newborns who were exposed to drugs, including heroin, in utero. Hyporeflexia, which refers to reduced or diminished reflexes, is one of the key findings in neonates experiencing NAS.
During pregnancy, when the mother uses opioids like heroin, the baby becomes dependent on the drug. After birth, when the drug is no longer available, the baby experiences withdrawal symptoms as the body adjusts to the absence of the drug. Hyporeflexia is a common manifestation of NAS and is observed due to the central nervous system's response to the withdrawal.
Let's go through the other options:
B. Frequent yawning: While yawning can be seen in neonates with NAS, it is not as specific to the condition as hyporeflexia. Yawning can occur for various reasons and may not always be indicative of NAS.
C. Respiratory depression: Respiratory depression can be a severe complication of opioid exposure in utero and can result in life-threatening situations for the neonate. However, it is not specific to NAS. Respiratory depression is more closely associated with opioid overdose in the newborn, which can be a separate concern from NAS.
D. Constipation: Constipation is a possible symptom in neonates experiencing NAS, but it is not as specific as hyporeflexia. Constipation can occur due to various factors and is not unique to NAS.
Correct Answer is B
Explanation
When caring for a client receiving heparin by continuous IV infusion for the treatment of venous thrombosis, the nurse should monitor the client's aPTT (Activated Partial Thromboplastin Time) to titrate the heparin dose.
Heparin is an anticoagulant medication used to prevent and treat blood clots. The aPTT is a coagulation test that measures the time it takes for the blood to clot when a specific activator is added. Monitoring the aPTT is a standard method for assessing the anticoagulant effect of heparin and ensuring that the client's blood remains within the desired therapeutic range.
The therapeutic range for aPTT while on heparin therapy varies depending on the indication and the client's condition but is generally maintained at a level that prolongs the clotting time enough to prevent and treat thrombosis while avoiding excessive bleeding risk.
Let's go through the other options:
A. Platelet function assay: While monitoring platelet function is essential for assessing overall hemostasis and platelet function, it is not specifically used for titrating heparin doses. Platelet function assays are more commonly used to assess the function of platelets in the context of platelet disorders or antiplatelet medication therapy.
C. INR (International Normalized Ratio): The INR is used to monitor the effect of vitamin K antagonist anticoagulants, such as warfarin, and is not the appropriate test for monitoring heparin therapy.
D. Amylase: Amylase is an enzyme produced by the pancreas and salivary glands and is not relevant for monitoring heparin therapy. Elevated amylase levels are typically associated with pancreatitis and not related to heparin treatment.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
