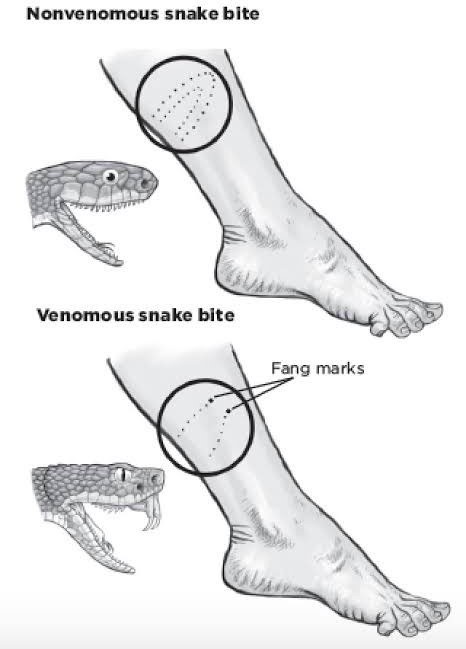
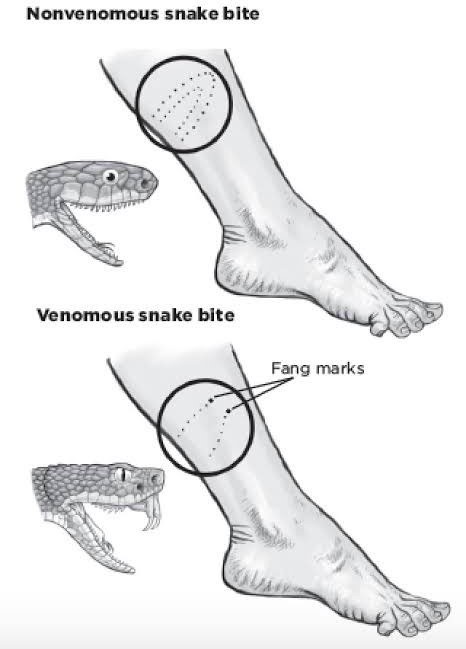
A nurse in an emergency department is assessing a client who was biten on the left leg by a poisonous snake. The client has placed elastic bandages snugly above and below the bite marks and is in no apparent distress. Which of the following actions should the nurse take?
Remove both of the elastic bandages from the leg.
Discharge the client.
Obtain a prescription for the appropriate anti-venom.
Obtain a prescription for pain medication.
The Correct Answer is C
Choice A: Removing the elastic bandages is not recommended. These bandages help slow the spread of venom by compressing the lymphatic vessels. Removing them could worsen the envenomation.
Choice B: This is incorrect. The nurse should not discharge the client, as they may develop serious complications from the snake bite, such as swelling, bleeding, infection, or shock. The client should be monitored closely and treated accordingly.
Choice C: This is the correct action. Antivenom treatment is crucial for serious snake envenomation. The sooner it can be administered, the better the outcome.
Choice D: While pain management is important, it is not the priority in this situation. Antivenom takes precedence over pain medication.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A: Removing the elastic bandages is not recommended. These bandages help slow the spread of venom by compressing the lymphatic vessels. Removing them could worsen the envenomation.
Choice B: This is incorrect. The nurse should not discharge the client, as they may develop serious complications from the snake bite, such as swelling, bleeding, infection, or shock. The client should be monitored closely and treated accordingly.
Choice C: This is the correct action. Antivenom treatment is crucial for serious snake envenomation. The sooner it can be administered, the better the outcome.
Choice D: While pain management is important, it is not the priority in this situation. Antivenom takes precedence over pain medication.
Correct Answer is B
Explanation
Choice A Reason: This is incorrect because the results are not within the expected reference range. The client's BUN, creatinine, and hematocrit are elevated, indicating dehydration or reduced renal perfusion.
Choice B Reason: This is correct because evaluating urine for amount and for specific gravity can help assess the client's hydration status and renal function. These actions can help assess the client's hydration status and renal function, which may be affected by nausea and vomiting. The client's BUN, creatinine, and hematocrit are elevated, indicating dehydration or reduced renal perfusion. The normal ranges for BUN are 7 to 20 mg/dL, for creatinine are
0.6 to 1.2 mg/dL, and for hematocrit are 38% to 50% for males. The nurse should monitor the urine output and specific gravity, which reflect the concentration and volume of urine. The normal range for urine output is 30 to 60 mL/hour, and for specific gravity is 1.005 to 1.030.
Choice C Reason: This is incorrect because collecting a urine specimen for culture and sensitivity is not indicated for this client. This action is used to diagnose urinary tract infections, which are not suggested by the client's symptoms or results.
Choice D Reason: This is incorrect because decreasing the IV fluid infusion rate and limiting oral fluid intake can worsen the client's dehydration and renal perfusion. The nurse should maintain adequate fluid intake and balance to prevent further complications.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
