A nurse assesses a patient’s peripheral IV site and notices edema and tenderness above the site. What action will the nurse take next?
Stop the infusion of IV fluids
Apply cold compresses to the IV site
Elevate the extremity on a pillow
Flush the catheter with normal saline
The Correct Answer is A
A. Stop the infusion of IV fluids:
This action may be appropriate if there are signs of infiltration or extravasation, where the IV fluid leaks into the surrounding tissue instead of entering the vein. Stopping the infusion can help prevent further tissue damage and assess the extent of the infiltration.
B. Apply cold compresses to the IV site:
Cold compresses can help reduce swelling and discomfort at the IV site. This action may be appropriate if there are signs of local inflammation or mild irritation at the insertion site.
C. Elevate the extremity on a pillow:
Elevating the extremity can help reduce swelling and promote venous return. This action is beneficial if there is edema or localized swelling above the IV site.
D. Flush the catheter with normal saline:
Flushing the catheter with normal saline is not typically the initial action in response to edema and tenderness above the IV site. Flushing is more commonly performed to ensure patency and proper functioning of the IV catheter.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
A.Prone positioning and postural drainage are typically not appropriate interventions for a client 1 day postoperative following an open thoracotomy, as this could place stress on the incision site and cause discomfort or injury.
B.High-Fowler's position facilitates lung expansion, which can improve ventilation and oxygenation. Encouraging the use of an incentive spirometer and promoting coughing helps clear secretions and expand the lungs, addressing the mild respiratory acidosis indicated by the ABG results (pH 7.31 and PaCO2 50 mm Hg).
C.Increasing oxygen to 70% is not appropriate, as the PaO2 level is within normal limits (93 mm Hg). The client's issue appears to be related more to ventilation (indicated by the elevated PaCO2) rather than oxygenation, so additional oxygen would not address the underlying cause and could lead to oxygen toxicity if used long-term.
D.A nonrebreather mask delivers a high concentration of oxygen, which is not necessary in this case since the client’s PaO2 is already adequate. The primary issue is not a lack of oxygen but rather the retention of CO2, so promoting ventilation and lung expansion through positioning and respiratory exercises is more appropriate.
Correct Answer is D
Explanation
A. Cardiac arrest related to septic shock:
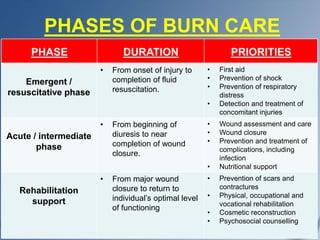
Septic shock can occur in burn patients due to the breakdown of the skin barrier, which allows pathogens to enter the bloodstream and cause systemic infection. However, while septic shock is a serious complication of burn injuries, it is not the primary cause of death in the emergent phase. Septic shock can lead to multiple organ failure and contribute to mortality, but it is often a later complication rather than an immediate cause in the emergent phase.
B. Infection:
Infections are a significant concern in burn patients, especially as the burn wound provides an ideal environment for bacterial growth. However, infections typically contribute more significantly to mortality in the later phases of burn care rather than in the emergent phase. In the emergent phase, hypovolemic shock and other immediate complications have a greater impact on mortality.
C. Adrenal failure:
Adrenal failure, specifically acute adrenal insufficiency or Addisonian crisis, can occur in burn patients due to the stress response and corticosteroid depletion. While adrenal insufficiency is a concern in severe burn cases, it is not the primary cause of death in the emergent phase requiring referral to a burn center.
D. Hypovolemic shock and renal failure:
Hypovolemic shock is a critical concern in the emergent phase of burn trauma because burns can lead to significant fluid loss and electrolyte imbalances. Hypovolemic shock results from insufficient circulating blood volume, leading to inadequate perfusion of organs and tissues, which can be life-threatening. Additionally, renal failure can develop due to hypovolemia, decreased cardiac output, and the release of inflammatory mediators, leading to acute kidney injury (AKI). Hypovolemic shock and subsequent renal failure are major contributors to mortality in the emergent phase of burn trauma, necessitating prompt referral to a burn center for specialized care.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
