A client with acute kidney injury is receiving hemodialysis.
Which of the following interventions should the nurse prioritize during the dialysis treatment?
Monitoring the client's blood pressure every 4 hours.
Administering a loop diuretic before the treatment.
Assessing the client's respiratory status every 2 hours.
Monitoring the client's electrolyte levels before and after the treatment.
Monitoring the client's electrolyte levels before and after the treatment.
The Correct Answer is D
Monitoring the client’s electrolyte levels before and after the treatment. This is because acute kidney injury (AKI) can cause electrolyte imbalances such as hyperkalemia, hyperphosphatemia, hypocalcemia, and metabolic acidosis. Hemodialysis can help correct these imbalances by removing excess fluid and waste products from the blood. However, hemodialysis can also cause electrolyte shifts and complications such as hypotension, muscle cramps, and arrhythmias. Therefore, it is important to monitor the client’s electrolyte levels before and after the treatment to assess the effectiveness and safety of hemodialysis.
Choice A is wrong because monitoring the client’s blood pressure every 4 hours is not frequent enough during hemodialysis.
Hemodialysis can cause rapid changes in blood pressure due to fluid removal and vascular access.
Therefore, blood pressure should be monitored more often, such as every 15 to 30 minutes during hemodialysis.
Choice B is wrong because administering a loop diuretic before the treatment is not indicated for AKI patients receiving hemodialysis.
Loop diuretics are used to increase urine output and reduce fluid overload in AKI patients who have some residual kidney function.
However, hemodialysis can achieve the same goal by removing excess fluid from the blood.
Moreover, loop diuretics can cause electrolyte depletion and ototoxicity, which can worsen the condition of AKI patients.
Choice C is wrong because assessing the client’s respiratory status every 2 hours is not specific enough for hemodialysis treatment.
Hemodialysis can affect respiratory mechanics by altering fluid balance, acid- base status, and oxygen delivery.
Therefore, respiratory status should be assessed more frequently and comprehensively during hemodialysis, such as by measuring respiratory rate, oxygen saturation, arterial blood gas, and chest auscultation.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
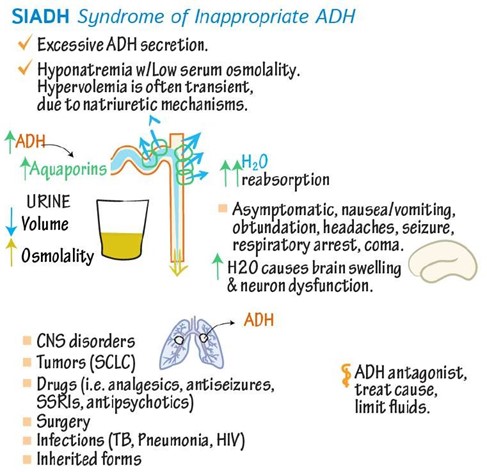
SIADH is a condition in which your body makes too much antidiuretic hormone (ADH), which controls how your body releases and conserves water.
SIADH makes it harder for your kidneys to release water and causes the levels of electrolytes, like sodium, to fall due to water retention.
This leads to hyponatremia, which is when you have low levels of sodium in your blood.
Choice B is wrong because hypernatremia is when you have high levels of sodium in your blood.
This can occur due to dehydration, excessive salt intake, or kidney problems.
Choice C is wrong because hyperkalemia is when you have high levels of potassium in your blood.
This can occur due to kidney failure, acidosis, or certain medications.
Choice D is wrong because hypokalemia is when you have low levels of potassium in your blood.
This can occur due to vomiting, diarrhea, diuretics, or alkalosis.
Correct Answer is A
Explanation
Clearance = urine flow rate x urine concentration / plasma concentration. This is the formula for calculating the renal clearance of a substance that is neither reabsorbed nor secreted by the tubules. Renal clearance is the volume of plasma that would have to be filtered by the glomeruli each minute to account for the amount of that substance appearing in the urine each minute.
Choice B is wrong because it has the urine concentration and plasma concentration inverted.
This would give an incorrect value for renal clearance.
Choice C is wrong because it has the plasma flow rate instead of the urine flow rate.
Plasma flow rate is not directly related to renal clearance.
Choice D is wrong because it has both the plasma flow rate and the urine concentration and plasma concentration inverted.
This would give an incorrect value for renal clearance.
Normal ranges for renal clearance vary depending on the substance, age, sex, and body size.
For example, the normal range for creatinine clearance is 85-125 mL/min for males and 75-115 mL/min for females.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
