A client with a newborn asks about the lesion on her child's head. After assessing the skin, which response will the nurse offer to the client?
This is a vascular tumor that often goes away over time
This lesion will spread
This is caused by scarring from the birth process
This is a precancerous lesion and your child will need a referral to a dermatologist
The Correct Answer is A
Choice A reason: This is correct because the lesion on the child's head is most likely a hemangioma, which is a benign tumor of blood vessels that appears as a red or purple mark on the skin. Hemangiomas are common in newborns and usually grow during the first year of life, then shrink and fade over several years. The nurse should reassure the client that hemangiomas are harmless and do not require treatment unless they interfere with vision, breathing, or feeding.
Choice B reason: This is incorrect because the lesion on the child's head will not spread, but rather grow and shrink within a limited area. The nurse should not alarm the client by suggesting that the lesion will spread to other parts of the body or become malignant. The nurse should explain that hemangiomas are not contagious or infectious and do not affect the child's overall health or development.
Choice C reason: This is incorrect because the lesion on the child's head is not caused by scarring from the birth process, but rather by abnormal growth of blood vessels in the skin. The nurse should not confuse or misinform the client about the cause of the lesion. The nurse should explain that hemangiomas are not related to trauma, infection, or genetics, but rather to unknown factors that influence blood vessel formation during fetal development.
Choice D reason: This is incorrect because the lesion on the child's head is not a precancerous lesion and does not need a referral to a dermatologist. The nurse should not scare or mislead the client by suggesting that the lesion is a sign of cancer or requires further evaluation or treatment. The nurse should explain that hemangiomas are benign and usually resolve on their own without any complications or sequelae.

Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
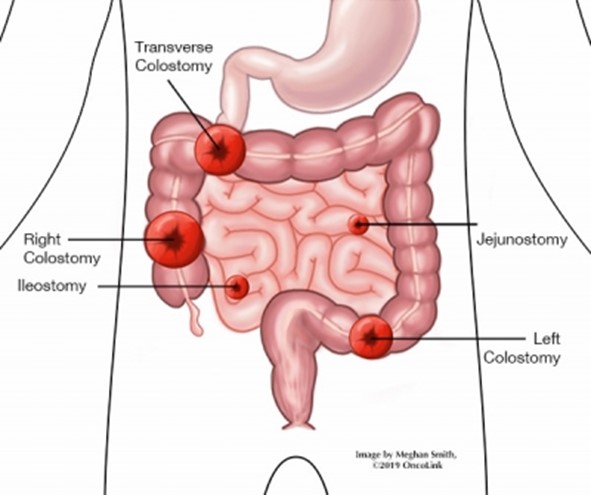
Choice A Reason: Soft pasty stool is normal for a transverse colostomy, as the stool has not reached the sigmoid colon where most of the water is absorbed.
Choice B Reason: This is the correct answer because purple discoloration of the stoma indicates ischemia or necrosis, which can lead to infection, perforation, or sepsis. It requires urgent intervention.
Choice C Reason: Stoma is beefy red is a normal finding for a healthy stoma, as it indicates adequate blood supply and healing.
Choice D Reason: There is skin excoriation around the stoma is a common complication of a colostomy, as the stool can irritate the skin. It can be managed with proper skin care and appliance fitting.
Correct Answer is D
Explanation
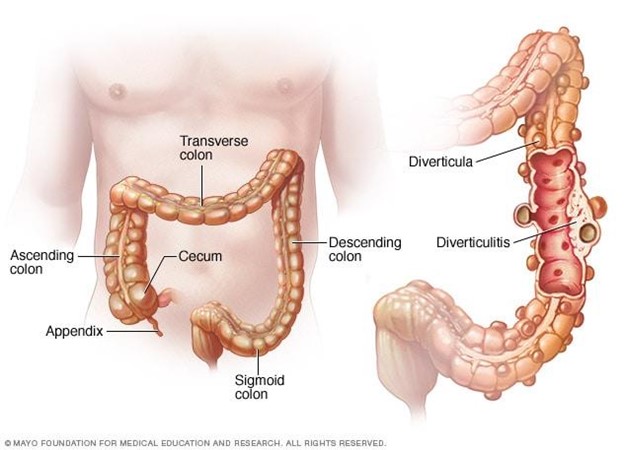
Choice A Reason: Increasing protein from red meat is not part of client education, as it can worsen the condition and increase the risk of complications. Red meat is high in fat and low in fiber, which can cause constipation and increase the pressure in the colon. Diverticulosis is a condition where small pouches or sacs form in the wall of the colon due to weak spots or increased pressure.
Choice B Reason: Decreasing fluid intake is not part of client education, as it can worsen the condition and increase the risk of complications. Fluid intake should be increased to prevent dehydration and promote bowel movements. Diverticulosis can cause abdominal pain, bloating, cramping, and changes in bowel habits.
Choice C Reason: Incorporating soft foods that are pureed in consistency is not part of client education, as it can worsen the condition and increase the risk of complications. Soft foods are low in fiber and can cause constipation and increase the pressure in the colon. Diverticulosis can lead to diverticulitis, which is inflammation or infection of the pouches or sacs.
Choice D Reason: This is the correct choice. Increasing dietary fiber is part of client education, as it can improve the condition and prevent complications. Fiber helps soften the stool and reduce the pressure in the colon. Diverticulosis can be managed by eating a high-fiber diet, drinking plenty of fluids, exercising regularly, and avoiding straining or holding stools.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
