A client newly diagnosed with glaucoma has a history of asthma. Which of the following medications newly prescribed by the eye doctor will the nurse question?
Antibiotics
Non-selective Beta Blockers
NSAIDs
Anticoagulants
The Correct Answer is B
Choice A Reason: Antibiotics are not contraindicated for a client with glaucoma and asthma, as they can treat or prevent infections that may affect the eye or the respiratory system.
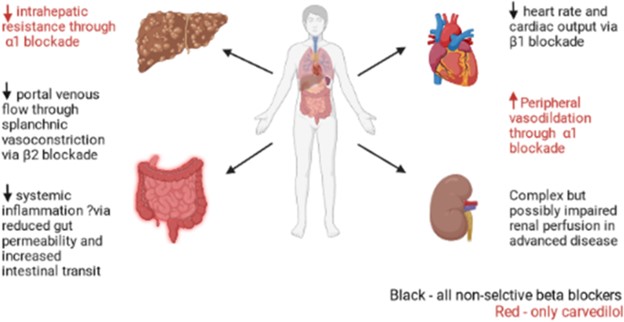
Choice B Reason: This is the correct answer because non-selective beta blockers are contraindicated for a client with glaucoma and asthma, as they can reduce intraocular pressure but also cause bronchoconstriction and exacerbate asthma symptoms.
Choice C Reason: NSAIDs are not contraindicated for a client with glaucoma and asthma, as they can reduce inflammation and pain that may affect the eye or the respiratory system.
Choice D Reason: Anticoagulants are not contraindicated for a client with glaucoma and asthma, as they can prevent or treat thromboembolic events that may affect the eye or the respiratory system.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A Reason: The burned area is yellow in color with severe edema is not a finding of a deep partial-thickness burn, but a superficial partial-thickness burn. A superficial partial-thickness burn involves the epidermis and the upper layer of the dermis, causing pain, redness, swelling, and blistering.
Choice B Reason: The burned area is black in color and pain is absent is not a finding of a deep partial-thickness burn, but a full-thickness burn. A full-thickness burn involves the epidermis, dermis, and underlying tissues, causing necrosis, charred skin, and loss of sensation.
Choice C Reason:This description aligns with a superficial partial-thickness (first-degree or mild second-degree) burn rather than a deep partial-thickness burn. Superficial partial-thickness burns involve the epidermis and the upper portion of the dermis. These burns appear pink or red, often accompanied by moisture and blister formation due to fluid leakage from damaged capillaries. They are painful because nerve endings remain intact. Healing occurs within 10 to 21 days without significant scarring.
Choice D Reason:Deep partial-thickness burns extend deeper into the dermis, damaging a larger portion of skin structures, including sweat glands and hair follicles. These burns typically appear red or white and may have a soft eschar (dead tissue), which differentiates them from more superficial burns that do not develop eschar. Unlike full-thickness burns, nerve endings remain partially intact, so the patient may still experience some pain. These burns take more than 21 days to heal and often require skin grafting to prevent complications such as contractures or hypertrophic scarring.
Correct Answer is C
Explanation
Choice A Reason: This is incorrect because rotating nursing staff may not provide emotional support for the client who is rehabilitating from major burns. The client may benefit from having consistent and familiar staff who can establish rapport and trust with him. The nurse should assign staff who are experienced and comfortable with burn care and who can communicate effectively and empathetically with the client.
Choice B Reason: This is incorrect because keeping family members aware of his condition may not provide emotional support for the client who is rehabilitating from major burns. The client may have privacy or confidentiality concerns or may not want his family members to see him in his current state. The nurse should respect the client's wishes and preferences regarding family involvement and obtain his consent before sharing any information.
Choice C Reason: This is correct because talking with the client during wound care can provide emotional support for the client who is rehabilitating from major burns. Wound care can be painful and stressful for the client, so the nurse should use therapeutic communication skills to distract, reassure, and encourage him. The nurse should also explain the procedures and rationale for wound care and allow the client to express his feelings and concerns.
Choice D Reason: This is incorrect because assigning assistive personnel to keep his room neat and clean may not provide emotional support for the client who is rehabilitating from major burns. The client may appreciate a clean environment, but he may also need more direct and personal contact with the nurse. The nurse should spend time with the client and provide holistic care that addresses his physical, psychological, social, and spiritual needs.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
