A client is reporting pain in her casted leg. The nurse has administered analgesics and elevated the limb. Thirty minutes after administering the analgesics. the client states the pain is unrelieved. The nurse is unable to palpate the client's dorsalis pedis or posterior tibial pulse and the client's foot is pale. The nurse suspects compartment syndrome. What is the nurse's most appropriate action?
Promptly inform the primary provider.
Reassess the client's neurovascular status in 15 minutes.
Warm the client's foot and determine whether circulation improves.
Reposition the client with the affected foot dependent.
The Correct Answer is A
Explanation:
A. Promptly inform the primary provider:
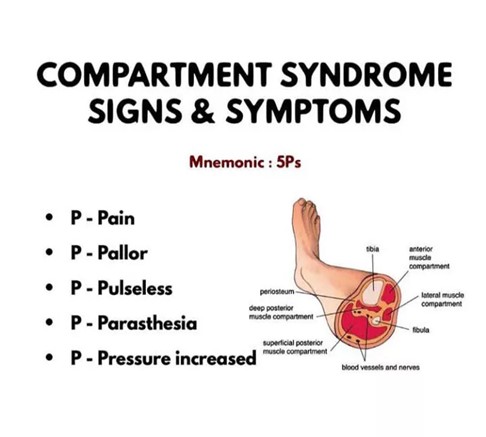
Explanation: Compartment syndrome is a medical emergency that requires immediate intervention. If a nurse suspects compartment syndrome due to symptoms like severe unrelieved pain, absent pulses, and pale extremities, the most appropriate action is to promptly inform the primary healthcare provider. The provider can assess the situation, order necessary diagnostic tests, and potentially arrange for emergent interventions like fasciotomy to relieve compartment pressure.
B. Reassess the client's neurovascular status in 15 minutes:
Explanation: Waiting for 15 minutes to reassess the client's neurovascular status is not appropriate in this situation. Compartment syndrome can progress rapidly, leading to irreversible tissue damage within a short time frame. Delaying assessment and intervention can result in significant complications.
C. Warm the client's foot and determine whether circulation improves:
Explanation: Warming the foot is not appropriate in this context. Compartment syndrome is caused by increased pressure within the muscle compartment, leading to compromised circulation. Warming the foot will not address the underlying issue of elevated compartment pressure and can potentially worsen the condition by dilating blood vessels and increasing pressure further.
D. Reposition the client with the affected foot dependent:
Explanation: Repositioning the client with the affected foot dependent is contraindicated in compartment syndrome. Elevating the limb can worsen the condition by further restricting blood flow. The limb should be kept at or slightly below the level of the heart to maintain adequate perfusion until medical intervention can be initiated.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
A. "I will reduce my intake of vitamin K-rich foods."
Vitamin K is essential for bone health as it helps in the regulation of calcium within bones and blood vessels. Therefore, reducing the intake of vitamin K-rich foods would not be beneficial for preventing osteoporosis. In fact, adequate intake of vitamin K is important for bone health.
B. "I will limit my intake of soft drinks." - Soft drinks, especially cola beverages, contain phosphoric acid, which can leach calcium from bones, making them weaker and more susceptible to fractures.
C. "I will reduce my intake of sodium." - High sodium intake can lead to increased calcium excretion in the urine, potentially weakening bones over time. Reducing sodium intake can help in preventing bone loss.
D. "I will decrease my intake of caffeine." - Excessive caffeine consumption can interfere with calcium absorption, contributing to bone loss. Decreasing caffeine intake is advisable for maintaining bone health.
Correct Answer is A
Explanation
A. Inadequate immobilization: Proper immobilization is essential for fractured bones to heal correctly. Immobilization, often achieved through casts, splints, or other orthopedic devices, stabilizes the broken bone fragments, allowing them to fuse back together. If the immobilization is not sufficient or if the patient doesn't follow the prescribed immobilization protocol, there can be excessive movement at the fracture site, hindering the healing process.
B. Venous thromboembolism: Venous thromboembolism (VTE) refers to the formation of blood clots in veins, usually in the legs (deep vein thrombosis) that can travel to the lungs (pulmonary embolism). While VTE is a potential complication after a fracture, it is not a direct cause of delayed bone union.
C. Inadequate vitamin D intake: Vitamin D is essential for bone health as it helps the body absorb calcium, which is crucial for bone formation and maintenance. Inadequate vitamin D levels can weaken bones and impair the healing process, but it's not a common cause of delayed bone union unless there are severe deficiencies or underlying medical conditions.
D. Bleeding at the injury site: Bleeding at the injury site occurs immediately after the fracture and is a natural part of the body's response to injury. While excessive bleeding can lead to complications, it is not a likely cause of delayed bone union six weeks after the injury. In the early stages of healing, bleeding is replaced by the formation of a hematoma, which eventually transforms into a callus and aids in the bone healing process.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
