A client is being admitted to the medical unit to rule out cardiac issues related to valve malfunction. Which question should the nurse ask the client during the admission interview to support this diagnosis?
“Did you have rheumatic fever as a child?”
“Do you have a family history of valve problems?”
“Do you have a history of MRSA?”
“What over-the-counter medications do you take?”
The Correct Answer is A
A. "Did you have rheumatic fever as a child?"
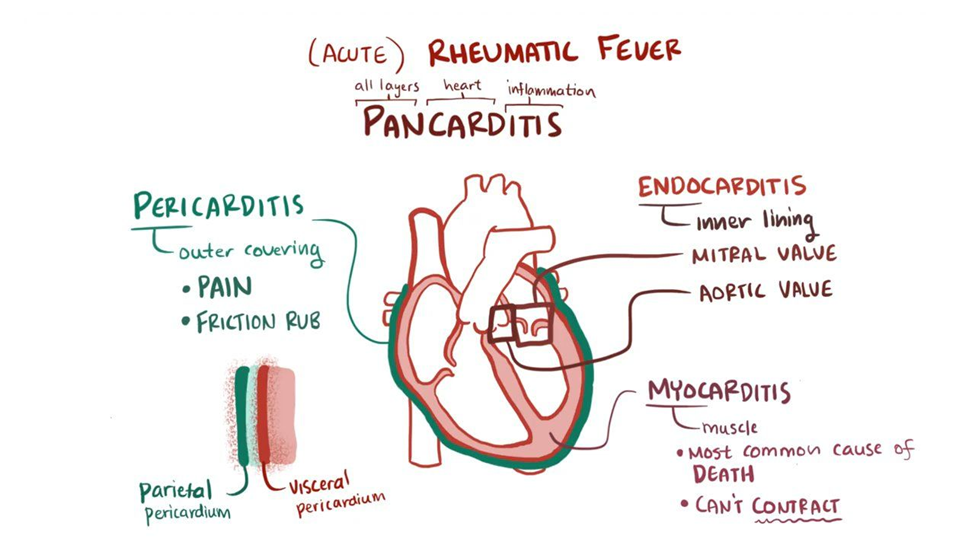
Rheumatic fever is an inflammatory condition that can affect the heart, especially the heart valves. Rheumatic fever is a known risk factor for the development of valvular heart disease. Asking about a history of rheumatic fever helps identify a potential cause for valve malfunction.
B. "Do you have a family history of valve problems?"
Family history can be relevant in understanding genetic predispositions to certain cardiac conditions. While it may contribute to the overall assessment of cardiac risk, it may not be as directly linked to valve malfunction as a history of rheumatic fever.
C. "Do you have a history of MRSA?"
MRSA (Methicillin-resistant Staphylococcus aureus) is a type of bacterial infection and is not directly associated with valve malfunction. This question may be relevant for other aspects of the client's health but is not specific to ruling out cardiac issues related to valve malfunction.
D. "What over-the-counter medications do you take?"
While knowing the medications a client takes is important for a comprehensive assessment, asking about over-the-counter medications may not be as directly related to ruling out cardiac issues related to valve malfunction. It is more relevant for assessing potential interactions or effects on cardiovascular health.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
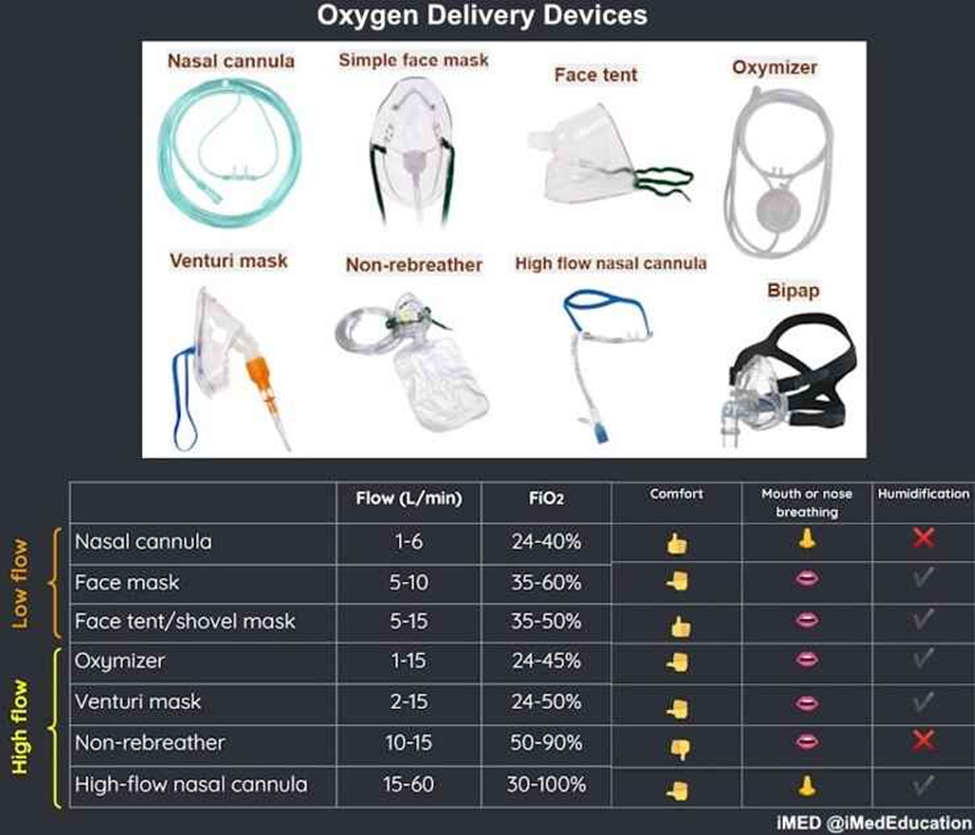
A. Partial non-rebreathing mask:
This mask delivers higher concentrations of oxygen than a nasal cannula. It has a reservoir bag that allows the client to rebreathe some exhaled air, increasing the oxygen concentration delivered. However, it may not be necessary for a client with mild shortness of breath and slightly reduced oxygen saturation.
B. Simple (Oxy Plus) mask:
The simple mask provides a higher concentration of oxygen than a nasal cannula but lacks the reservoir bag found in the non-rebreathing mask. It is generally used for moderate oxygen needs. However, it might be more than what is required for a client with mild shortness of breath and slightly reduced oxygen saturation.
C. Nasal cannula:
Nasal cannulas are commonly used for clients with mild respiratory distress. They deliver a lower to moderate concentration of oxygen and are well-tolerated by most clients. They are suitable for individuals with mild shortness of breath and can be adjusted based on the required flow rate.
D. Non-rebreathing mask:
The non-rebreathing mask provides the highest concentration of oxygen among the options listed. It includes a reservoir bag to deliver a higher oxygen concentration. It is typically reserved for clients with higher oxygen requirements. For a client with mild shortness of breath and slightly reduced oxygen saturation, this may be more than necessary.
Correct Answer is B
Explanation
A. Intermittent claudication:
Intermittent claudication is more commonly associated with peripheral arterial insufficiency rather than venous insufficiency. It is caused by inadequate blood flow to the muscles during activity, resulting in cramping or pain that typically resolves with rest.
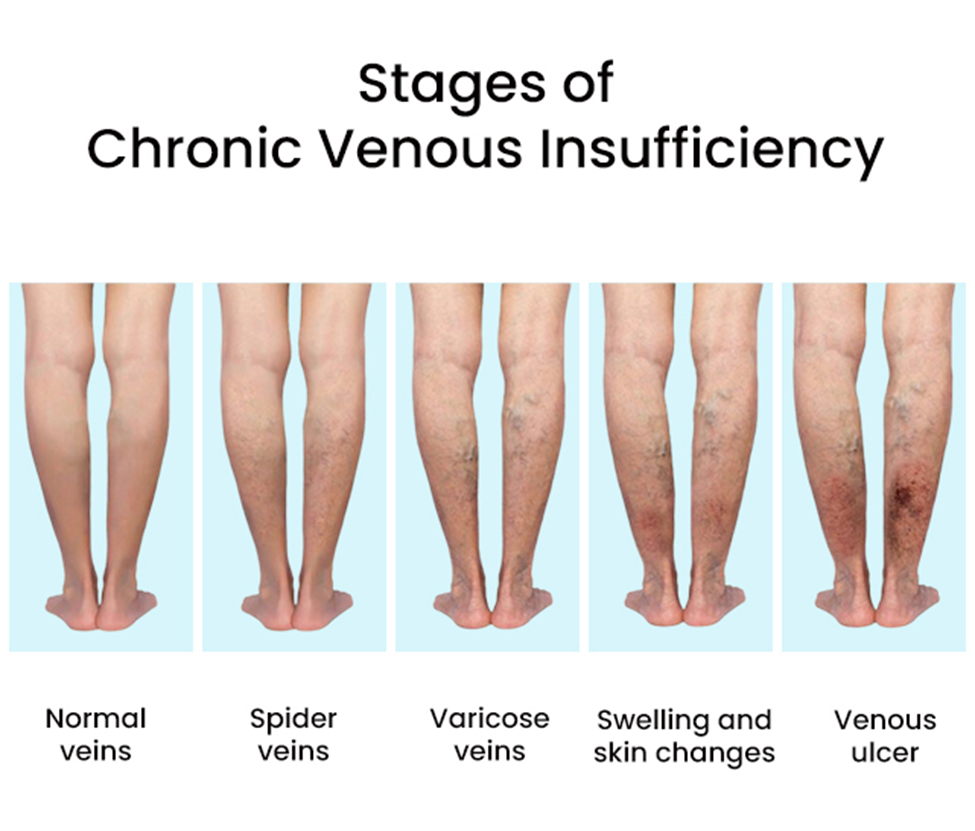
B. Brownish discoloration to the legs:
Brownish discoloration to the legs, often referred to as hemosiderin staining, is a common finding in peripheral venous insufficiency. It occurs due to the breakdown of red blood cells and the deposition of hemosiderin in the tissues, especially around the ankles.
C. Weak or absent pedal pulses:
Weak or absent pedal pulses are more indicative of peripheral arterial insufficiency rather than venous insufficiency. Peripheral arterial disease can result in decreased blood flow to the extremities, leading to diminished pulses.
D. Unequal peripheral pulses between extremities:
Unequal peripheral pulses between extremities are also more suggestive of arterial insufficiency. Conditions such as atherosclerosis or arterial embolism can cause variations in pulses between different limbs.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
