A 25-year-old gravida 1 para 1 who had an emergency cesarean birth 3 days ago is scheduled for discharge. As the nurse prepares her for discharge, she begins to cry. What action should the nurse take first?
Point out how lucky she is to have a healthy baby
Assess her for pain
Explain that she is experiencing postpartum blues
Allow her time to express her feelings
The Correct Answer is D
Choice A: This is incorrect because pointing out how lucky she is to have a healthy baby may invalidate her feelings and make her feel guilty or ashamed. The nurse should acknowledge and respect the client's emotions and avoid making judgments or comparisons.
Choice B: This is incorrect because assessing her for pain is not the first action that the nurse should take. Although pain may be a factor that contributes to the client's emotional state, it is not the primary cause of her crying. The nurse should first establish rapport and trust with the client and then assess her physical and psychological needs.
Choice C: This is incorrect because explaining that she is experiencing postpartum blues may be premature and inaccurate. Postpartum blues are mild and transient mood changes that occur in up to 80% of women within the first few days after childbirth. They are characterized by tearfulness, irritability, anxiety, and mood swings. However, the nurse should not assume that the client has postpartum blues without performing a thorough assessment and ruling out other possible causes of her crying, such as postpartum depression, anxiety, or trauma.
Choice D: This is the correct answer because allowing her time to express her feelings is the most appropriate and empathetic action that the nurse should take first. The nurse should listen actively and attentively to the client and provide emotional support and reassurance. The nurse should also use open-ended questions and reflective statements to facilitate communication and explore the client's concerns and coping strategies.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A) Maternal blood type is correct because this is an essential and relevant information for the nurse to check for a woman who has had a first trimester spontaneous abortion. Spontaneous abortion, also known as miscarriage, is the loss of pregnancy before 20 weeks of gestation. It can be caused by various factors such as chromosomal abnormalities, infections, trauma, or hormonal imbalances. Maternal blood type is the classification of blood based on the presence or absence of antigens and antibodies on the red blood cells and plasma. The most common blood types are A, B, AB, and O, and each can be positive or negative for the Rh factor. Checking maternal blood type can help to identify and prevent Rh incompatibility, which is a condition that occurs when the mother has Rh-negative blood and the fetus has Rh-positive blood. This can cause the mother's immune system to produce antibodies that attack the fetal red blood cells, leading to hemolytic disease of the fetus and newborn (HDFN), which can cause anemia, jaundice, or death. To prevent this, the nurse should administer Rh immunoglobulin (RhoGAM) to the mother within 72 hours after a spontaneous abortion or any event that may cause mixing of maternal and fetal blood. Therefore, this information is vital and appropriate for the nurse to check.
Choice B) Past obstetric history is incorrect because this is not an essential or urgent information for the nurse to check for a woman who has had a first trimester spontaneous abortion. Past obstetric history is the record of previous pregnancies and their outcomes, such as number, duration, complications, or interventions. It can provide useful information for assessing the risk factors and health status of the current pregnancy. However, it does not have any immediate impact or implication for the management of a spontaneous abortion, which is a common and unpredictable event that affects about 10% to 20% of all pregnancies. Therefore, this information can be obtained later or from other sources by the nurse.
Choice C) Maternal varicella titer is incorrect because this is not a relevant or necessary information for the nurse to check for a woman who has had a first trimester spontaneous abortion. Varicella titer is a blood test that measures the level of antibodies against varicella-zoster virus (VZV), which causes chickenpox and shingles. It can indicate whether a person has immunity to VZV or needs vaccination. Checking maternal varicella titer may be important for pregnant women who have not had chickenpox or vaccination before, as VZV infection during pregnancy can cause congenital varicella syndrome (CVS), which can affect the development and function of various organs in the fetus. However, it does not relate to spontaneous abortion, which is not caused by VZV infection or immunity. Therefore, this information is irrelevant and unnecessary for the nurse to check.
Choice D) Cervical patency is incorrect because this is not a reliable or accurate information for the nurse to check for a woman who has had a first trimester spontaneous abortion. Cervical patency means how open or closed the cervix is, which can affect the progress and outcome of labor and delivery. The cervix is usually closed and firm during pregnancy, but it gradually softens, shortens, and dilates as labor approaches. Checking cervical patency can help to determine if labor has started or if there are any complications such as preterm labor or cervical incompetence.
However, it does not indicate if a spontaneous abortion has occurred or not, as the cervix may remain closed or partially open after a miscarriage. Moreover, checking cervical patency can be invasive and uncomfortable for the woman who has had a spontaneous abortion, and it may increase the risk of infection or bleeding. Therefore, this information should be checked only when indicated by the physician and with caution by the nurse.

Correct Answer is B
Explanation
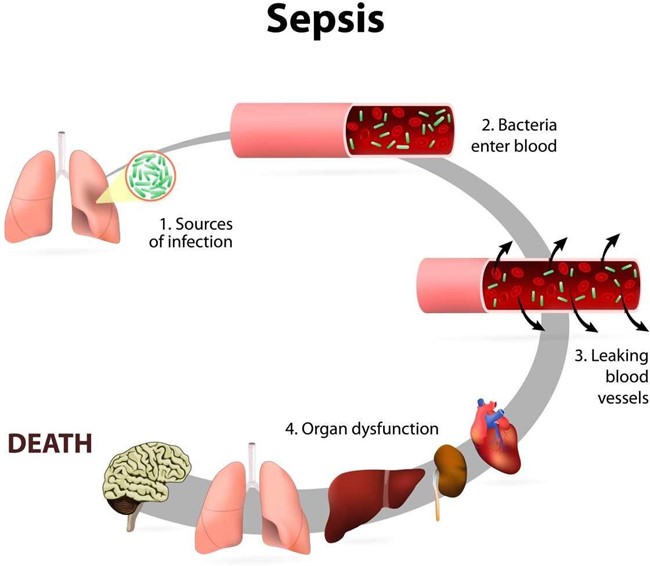
Choice A) Increased urinary output: This is not a sign of sepsis in newborns. In fact, sepsis can cause reduced urinary output due to poor blood flow to the kidneys and dehydration.
Choice B) Hypothermia: This is a sign of sepsis in newborns. Sepsis can cause changes in temperature, often fever, but sometimes low temperature. Hypothermia can indicate a severe infection that affects the body's ability to regulate its temperature.
Choice C) Wakefulness: This is not a sign of sepsis in newborns. Sepsis can cause reduced activity and lethargy due to inflammation and organ dysfunction.
Choice D) Interest in feeding: This is not a sign of sepsis in newborns. Sepsis can cause reduced sucking and difficulty feeding due to poor appetite, nausea, vomiting, and abdominal distension.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
