Types of Oxygen Delivery Devices
- Oxygen delivery devices are classified into low-flow and high-flow systems, depending on whether they provide a fixed or variable amount of oxygen to the patient.
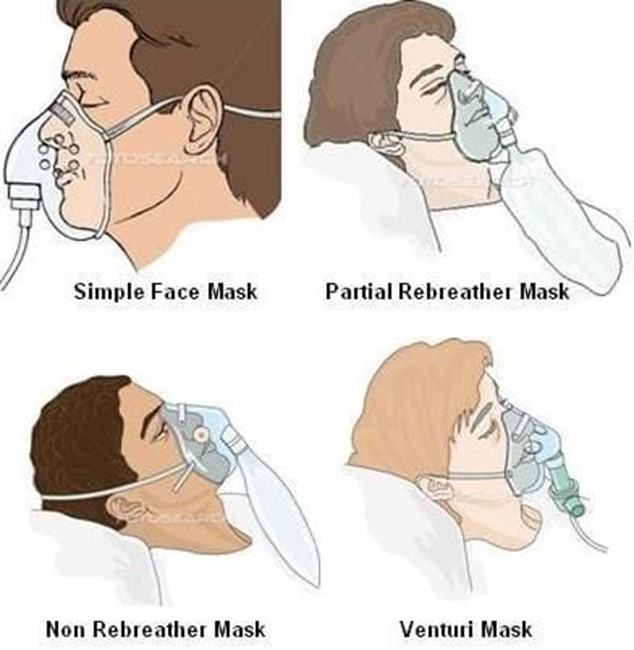
- Low-flow systems deliver a variable amount of oxygen that depends on the patient’s breathing pattern and rate. They include a nasal cannula, simple face mask, partial rebreather mask, and non-rebreather mask.
- High-flow systems deliver a fixed amount of oxygen that is independent of the patient’s breathing pattern and rate. They include a venturi mask, aerosol mask, face tent, tracheostomy collar, T-piece, and mechanical ventilator.
- The table below summarizes the characteristics, advantages, disadvantages, and nursing implications of each type of oxygen delivery device.
|
Device
|
FiO2 range
|
Flow rate
|
Characteristics
|
Advantages
|
Disadvantages
|
Nursing implications |
|
Nasal cannula
|
24%-44%
|
1-6 L/min
|
A plastic tubing with two prongs that fit into the nostrils.
|
Comfortable, easy to apply, well-tolerated by most patients.
|
Can cause nasal dryness, irritation, or bleeding. Can be dislodged by movement or mouth breathing. FiO2 can vary with breathing pattern.
|
Assess nares for patency and skin integrity. Humidify oxygen if flow rate is higher than 4 L/min. Ensure proper fit and secure tubing. Monitor for signs of hypoxia or hypercarbia. |
|
Simple face mask
|
40%-60%
|
5-8 L/min
|
A plastic mask that covers the nose and mouth. Has holes on the sides to allow exhaled air to escape.
|
Easy to apply and remove. Provides higher FiO2 than nasal cannula. Humidifies oxygen.
|
Can cause skin irritation, pressure ulcers, or claustrophobia. Can interfere with eating, drinking, or talking. FiO2 can vary with breathing pattern. Risk of aspiration if vomiting occurs.
|
Assess skin integrity and comfort. Ensure proper fit and secure straps. Monitor for signs of hypoxia or hypercarbia. Provide oral care every 2-4 hours. Remove mask for eating or drinking. |
|
Partial rebreather mask
|
60%-75%
|
6-11 L/min
|
A plastic mask that covers the nose and mouth. Has a reservoir bag attached to store oxygen-enriched air. Has holes on the sides to allow some exhaled air to escape and some to be rebreathed.
|
Provides higher FiO2 than simple face mask. Allows conservation of oxygen by rebreathing some exhaled air. Humidifies oxygen.
|
Same as simple face mask plus risk of suffocation if bag deflates or collapses. FiO2 can vary with breathing pattern and bag inflation. Requires close monitoring.
|
Same as simple face mask plus ensure bag remains inflated during inspiration and expiration. Adjust flow rate to prevent bag collapse. Monitor for signs of hypoxia or hypercarbia. |
|
Non-rebreather mask
|
80%-95%
|
10-15 L/min
|
A plastic mask that covers the nose and mouth. Has a reservoir bag attached to store 100% oxygen. Has one-way valves on the mask and bag to prevent exhaled air from entering the bag or being rebreathed. Has holes on the sides to allow exhaled air to escape completely.
|
Provides highest FiO2 among low-flow systems. Prevents rebreathing of exhaled air and carbon dioxide. Humidifies oxygen.
|
Same as partial rebreather mask plus risk of carbon dioxide retention if valves malfunction. Requires close monitoring.
|
Same as partial rebreather mask plus ensure valves are patent and functional. Monitor for signs of hypoxia or hypercarbia. |
|
Venturi mask
|
24%-50%
|
4-12 L/min
|
A plastic mask that covers the nose and mouth. Has a cone-shaped adapter (venturi) attached to the oxygen source. Has holes on the sides to allow room air to mix with oxygen. The FiO2 is determined by the size and color of the adapter.
|
Provides precise and consistent FiO2 regardless of breathing pattern. Allows control of oxygen concentration and humidity.
|
Can cause skin irritation, pressure ulcers, or claustrophobia. Can interfere with eating, drinking, or talking. Risk of aspiration if vomiting occurs. Requires careful monitoring and maintenance.
|
Assess skin integrity and comfort. Ensure proper fit and secure straps. Monitor for signs of hypoxia or hypercarbia. Provide oral care every 2-4 hours. Remove mask for eating or drinking. Check adapter size and color and flow rate according to prescription. Ensure adequate water level in humidifier. |
|
Aerosol mask
|
24%-100%
|
8-15 L/min
|
A plastic mask that covers the nose and mouth or the entire face. Has a large-bore tubing connected to an aerosol generator that produces a mist of oxygen and water particles. The FiO2 is determined by the flow rate and the amount of mist generated.
|
Provides high FiO2 and humidity for patients with thick secretions, dry mucous membranes, or upper airway edema. Can be used for patients who cannot tolerate masks or nasal cannula.
|
Can cause skin irritation, pressure ulcers, or claustrophobia. Can interfere with eating, drinking, or talking. Risk of aspiration if vomiting occurs. Requires careful monitoring and maintenance. Can be noisy and messy.
|
Same as venturi mask plus ensure adequate water level in aerosol generator. Check tubing for condensation and drainage. Monitor for signs of infection or fluid overload. |
|
Face tent
|
24%-100%
|
8-15 L/min
|
A soft plastic cone that fits loosely around the face and neck. Has a large-bore tubing connected to an aerosol generator that produces a mist of oxygen and water particles. The FiO2 is determined by the flow rate and the amount of mist generated.
|
Same as aerosol mask plus more comfortable and less confining than masks.
|
Same as aerosol mask plus less precise and consistent FiO2 than masks.
|
Same as aerosol mask plus ensure proper fit and secure straps. |
|
Device
|
FiO2
|
Flow rate
|
Description
|
Advantages
|
Disadvantages
|
Nursing considerations |
|
Tracheostomy collar
|
24%-100%
|
8-15 L/min
|
A plastic collar that fits around the neck and covers the tracheostomy opening. Has a large-bore tubing connected to an aerosol generator that produces a mist of oxygen and water particles. The FiO2 is determined by the flow rate and the amount of mist generated.
|
Same as aerosol mask plus provides direct oxygen delivery to the trachea. Can be used for patients who have a tracheostomy or laryngectomy.
|
Same as aerosol mask plus risk of infection, bleeding, or obstruction of the tracheostomy site. Requires careful monitoring and maintenance. Can be noisy and messy.
|
Same as aerosol mask plus assess tracheostomy site for patency, cleanliness, and signs of infection. Provide tracheostomy care every 8 hours or as needed. Suction secretions as needed. Monitor for signs of hypoxia or hypercarbia. |
|
T-piece
|
24%-100%
|
8-15 L/min
|
A plastic adapter that connects to the end of a tracheostomy tube, endotracheal tube, or laryngectomy tube. Has a large-bore tubing connected to an aerosol generator that produces a mist of oxygen and water particles. The FiO2 is determined by the flow rate and the amount of mist generated.
|
Same as tracheostomy collar plus allows the patient to breathe room air when disconnected from the oxygen source. Can be used for patients who are being weaned from mechanical ventilation or have intermittent suctioning needs.
|
Same as tracheostomy collar plus risk of accidental disconnection or loss of oxygen supply. Requires careful monitoring and maintenance. Can be noisy and messy.
|
Same as tracheostomy collar plus ensure proper fit and secure connection. Monitor for signs of hypoxia or hypercarbia. Disconnect from oxygen source only when ordered or indicated. |
|
Mechanical ventilator
|
21%-100%
|
Variable
|
A machine that delivers oxygen and air to the lungs through a tracheostomy tube or an endotracheal tube. The FiO2, tidal volume, respiratory rate, inspiratory pressure, positive end-expiratory pressure (PEEP), and other parameters are set by the health care provider according to the patient’s condition and needs.
|
Provides precise and consistent FiO2 and ventilation for patients who cannot breathe adequately on their own. Allows control of oxygen concentration, humidity, temperature, and pressure. Can provide various modes of ventilation, such as assist-control, synchronized intermittent mandatory ventilation (SIMV), pressure support ventilation (PSV), etc.
|
Can cause complications such as barotrauma, volutrauma, atelectrauma, ventilator-associated pneumonia (VAP), ventilator-induced lung injury (VILI), etc. Requires invasive intubation or tracheostomy and sedation or paralysis for some patients. Requires careful monitoring and maintenance by trained personnel. Can be noisy and complex.
|
Assess respiratory status and ventilator settings frequently. Monitor ABG results and pulse oximetry readings. Ensure proper placement and securement of the artificial airway. Provide oral care every 2-4 hours or as needed. Suction secretions as needed. Prevent accidental extubation or disconnection. Monitor for signs of infection, bleeding, or obstruction of the artificial airway. Monitor for signs of hypoxia, hypercarbia, or ventilator complications. |
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Questions on Types of Oxygen Delivery Devices
Correct Answer is B
Explanation
Correct Answer is ["A","B","D"]
Explanation
Correct Answer is C
Explanation
Correct Answer is B
Explanation
Correct Answer is B
Explanation
Correct Answer is D
Explanation
Correct Answer is C
Explanation
Correct Answer is ["B","C","D"]
Explanation
Correct Answer is A
Explanation
Correct Answer is ["A","C","E"]
Explanation
Correct Answer is B
Explanation
Search Here
Related Topics
More on Nursing
Free Nursing Study Materials
Access to all study guides and practice questions for nursing for free.
- Free Nursing Study Trials
- Free Nursing Video tutorials
- Free Nursing Practice Tests
- Free Exam and Study Modes
- Free Nursing Revision Quizlets

