Management and Treatment
- The management and treatment of peritonitis depend on the cause, severity, and complications of the condition.
- The main goals are to control the infection, correct the fluid and electrolyte imbalance, relieve the pain and discomfort, and prevent further complications.
- The following are some of the interventions that may be implemented:
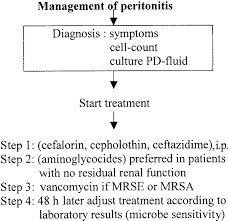
- Antibiotics- Antibiotics are administered to treat the infection and prevent sepsis. The choice of antibiotics depends on the source and type of infection, as well as the susceptibility of the organism. Broad-spectrum antibiotics are usually started empirically until the culture results are available. The duration of antibiotic therapy may vary from 7 to 14 days or longer depending on the response and resolution of the infection.
- Fluid resuscitation- Fluid resuscitation is initiated to restore the fluid volume and correct the dehydration and hypovolemia caused by peritonitis. Intravenous (IV) fluids such as normal saline or lactated Ringer's solution are given to replace the fluid losses and maintain adequate urine output and blood pressure. The amount and type of fluids are adjusted based on the patient's condition and laboratory results.
- Analgesics- Analgesics are given to relieve the pain and discomfort associated with peritonitis. Opioids such as morphine or fentanyl are commonly used for moderate to severe pain. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or ketorolac may be used for mild to moderate pain. However, NSAIDs should be used with caution in patients with renal impairment or bleeding disorders.
- Surgical intervention- Surgical intervention may be required to remove the source of infection or perforation, drain the abscess or fluid collection, repair the damaged tissue or organ, or perform a bowel resection or ostomy if necessary. The type and extent of surgery depend on the cause and severity of peritonitis.
Nursing Test Bank
Quiz #1: RN Exams Pharmacology Exams
Quiz #2: RN Exams Medical-Surgical Exams
Quiz #3: RN Exams Fundamentals Exams
Quiz #4: RN Exams Maternal-Newborn Exams
Quiz #5: RN Exams Anatomy and Physiology Exams
Quiz #6: RN Exams Obstetrics and Pediatrics Exams
Quiz #7: RN Exams Fluid and Electrolytes Exams
Quiz #8: RN Exams Community Health Exams
Quiz #9: RN Exams Promoting Health across the lifespan Exams
Quiz #10: RN Exams Multidimensional care Exams
Naxlex Comprehensive Predictor Exams
Quiz #1: Naxlex RN Comprehensive online practice 2019 B with NGN
Quiz #2: Naxlex RN Comprehensive Predictor 2023
Quiz #3: Naxlex RN Comprehensive Predictor 2023 Exit Exam A
Quiz #4: Naxlex HESI Exit LPN Exam
Quiz #5: Naxlex PN Comprehensive Predictor PN 2020
Quiz #6: Naxlex VATI PN Comprehensive Predictor 2020
Quiz #8: Naxlex PN Comprehensive Predictor 2023 - Exam 1
Quiz #10: Naxlex HESI PN Exit exam
Quiz #11: Naxlex HESI PN EXIT Exam 2
Questions on Management and Treatment
Correct Answer is C
Explanation
Diverticulitis is inflammation of the diverticula (small pouches) in the colon and is not related to a ruptured appendix.
Correct Answer is D
Explanation
Sudden-onset severe abdominal pain and tenderness are classic early signs of peritonitis and indicate the need for immediate medical attention.
Correct Answer is C
Explanation
A CBC may show elevated white blood cell count, which is an indication of infection, but it is not a confirmatory test for peritonitis.
Correct Answer is C
Explanation
Bradycardia is not a common side effect of IV antibiotic therapy.
Correct Answer is B
Explanation
Monitoring intra-abdominal pressure is not the purpose of a paracentesis.
Correct Answer is A
Explanation
Bowel rest may be indicated for other conditions but is not the primary intervention for SBP.
Correct Answer is A
Explanation
Constipation may cause abdominal distension, but decreased bowel sounds are not characteristic of constipation.
Correct Answer is D
Explanation
Rapid, shallow breathing is a common early sign of septic shock and indicates the body's attempt to compensate for the decreased cardiac output.
Correct Answer is C
Explanation
A vegetarian diet is not a risk factor for peritonitis.
Correct Answer is D
Explanation
A history of inflammatory bowel disease is a significant risk factor for peritonitis, especially if there are complications such as bowel perforation.
Correct Answer is B
Explanation
GERD is not a risk factor for peritonitis.
Correct Answer is B
Explanation
Chronic lung disease is not directly related to peritonitis.
Correct Answer is C
Explanation
Oral contraceptives do not increase the risk of developing peritonitis.
Correct Answer is A
Explanation
An allergic reaction to the dialysis solution is a possibility but is not the primary reason for an increased risk of peritonitis in clients undergoing peritoneal dialysis.
Correct Answer is C
Explanation
Frequent use of antacids may alleviate symptoms of gastric ulcers but is not directly related to an increased risk of peritonitis in clients with perforated gastric ulcers.
Correct Answer is B
Explanation
Reduced gastrointestinal motility is a normal age-related change but is not directly related to an increased susceptibility to peritonitis in older adults.
Correct Answer is C
Explanation
Shortness of breath is not a common symptom of peritonitis unless there is an associated respiratory complication.
Correct Answer is D
Explanation
The client's elevated temperature, rapid heart rate, and shallow breathing are indicative of a systemic inflammatory response, which is a characteristic feature of peritonitis.
Correct Answer is D
Explanation
The finding of a rigid, board-like abdomen upon palpation is known as guarding, which is a protective response of the abdominal muscles in peritonitis to minimize movement and protect the inflamed peritoneum.
Correct Answer is B
Explanation
Radiating pain is pain that extends from its source to other areas, and it is not specifically described in the scenario.
Correct Answer is B
Explanation
Urinary retention involves the inability to empty the bladder fully and is not related to the findings described in the scenario.
Correct Answer is B
Explanation
Dehydration may result in elevated blood cell counts due to hemoconcentration, but it is not the primary cause of an elevated white blood cell count in peritonitis.
Correct Answer is C
Explanation
Respiratory distress is not directly related to the findings described in the scenario.
Correct Answer is C
Explanation
Renal failure involves impaired kidney function and may present with specific signs, but it is not directly related to the signs described in the scenario.
An abdominal computed tomography (CT) scan is a valuable diagnostic tool for identifying signs of inflammation and infection in the peritoneal cavity, aiding in the confirmation of peritonitis.
Taking a tissue sample from the peritoneal lining is not the purpose of diagnostic paracentesis.
Ultrasonography can provide images of the abdominal organs, but it may not offer the level of detail provided by MRI in assessing peritonitis.
An elevated white blood cell count (WBC) is a common finding in peritonitis, indicating an inflammatory response and possible infection in the peritoneal cavity.
Hyperactive bowel sounds may occur with gastrointestinal disorders but are not specific to peritonitis.
Pancreatitis is inflammation of the pancreas and may cause abdominal pain, but it is not associated with generalized bloating and distension of the abdomen.
Evaluating lung health would involve pulmonary imaging, not the imaging indicated for peritonitis.
Removal of fluid from the spinal canal would be a lumbar puncture, not a paracentesis.
Encouraging deep breathing and coughing exercises is beneficial for preventing respiratory complications, but it is not the highest priority compared to addressing the infection with antibiotics.
Implementing fall precautions is important for clients at risk of falls, but it is not directly related to potential complications of peritonitis.
Administering prescribed analgesics is essential for managing the client's pain and providing comfort during the treatment of peritonitis.
Administering the antibiotics through a peripheral IV catheter may not be suitable for the client's condition, as peritonitis may necessitate the use of a central line for administration of IV medications.
Promoting bowel rest is the main purpose of continuous gastric suction in the management of peritonitis. By reducing the workload of the gastrointestinal tract, the inflamed peritoneum can heal and recover more effectively.
Restoring fluid balance is a goal of fluid resuscitation, but the primary focus is on preventing circulatory collapse and ensuring adequate tissue perfusion.
Diarrhea is not
a common side effect of opioid use in clients with peritonitis.
Using a heating pad for abdominal pain relief may not be recommended for all clients recovering from peritonitis, as it may exacerbate inflammation or lead to complications. Individualized pain management strategies should be discussed with the healthcare provider.
Providing deep breathing exercises is important for preventing respiratory complications, but it is not the highest priority compared to addressing sepsis with antibiotics.
Mild incisional pain is expected after surgery, but it does not indicate the development of abdominal compartment syndrome.
Maintaining fluid and electrolyte balance is crucial in managing acute kidney injury in peritonitis. The nurse should closely monitor the client's fluid intake, output, and electrolyte levels and collaborate with the healthcare team to adjust the fluid therapy as needed.
Gastrointestinal bleeding may present with symptoms such as melena or hematemesis but is not directly associated with hypotension and tachycardia.
Administering enteral nutrition may be a secondary purpose of an NG tube in some cases, but it is not the primary goal in clients with peritonitis.
Administering bronchodilator medication is not the priority intervention in managing acute respiratory distress unless there is a specific indication for its use.
<p>Increased urine output may be a positive finding but does not directly relate to the development of hypovolemic shock.</p>
<p>Providing pain medication as needed is important for the client's comfort but does not directly prevent the spread of infection.</p>
Search Here
Related Topics
More on Nursing
Free Nursing Study Materials
Access to all study guides and practice questions for nursing for free.
- Free Nursing Study Trials
- Free Nursing Video tutorials
- Free Nursing Practice Tests
- Free Exam and Study Modes
- Free Nursing Revision Quizlets
