Complications and Interventions
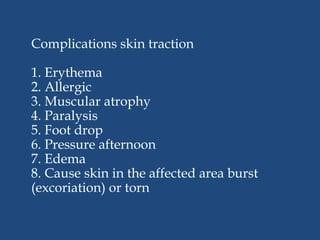
Complications of Skin Traction:
- Skin Breakdown: Prolonged application of skin traction can lead to pressure and friction on the skin, resulting in skin breakdown, pressure ulcers, or open sores.
- Circulatory Compromise: Improperly applied or excessively tight traction may impede blood flow, leading to circulatory compromise, ischemia, and tissue damage.
- Nerve Compression: Traction forces may compress nerves, leading to neuropathy, numbness, tingling, or loss of sensation in the affected limb.
- Joint Stiffness: Extended immobilization in traction can contribute to joint stiffness, contractures, and decreased range of motion.
- Muscle Atrophy: Prolonged immobility and reduced weight-bearing can cause muscle wasting and weakness in the affected limb.
Interventions to Prevent Complications:
- Regular Repositioning: Reposition the patient regularly to relieve pressure on bony prominences and distribute weight evenly on the skin.
- Skin Assessment: Perform frequent skin assessments to identify areas of pressure or early signs of skin breakdown. Provide appropriate skin care and ensure the skin is clean and dry.
- Padding and Pressure-Relieving Devices: Use foam padding or pressure-relieving devices under bony prominences to minimize pressure and protect the skin.
- Adequate Traction Setup: Ensure that the traction apparatus is correctly set up, and weights hang freely without touching the floor, reducing the risk of traction-related complications.
- Neurovascular Checks: Perform regular neurovascular checks to assess circulation, sensation, and motor function of the affected limb. Report any changes in neurovascular status promptly.
- Encourage Mobility: Encourage active and passive range-of-motion exercises for unaffected limbs to maintain joint mobility and prevent muscle atrophy.
- Educate Patients and Families: Educate the patient and family about the importance of maintaining proper body alignment, adhering to prescribed traction parameters, and promptly reporting any concerns or complications.
Nursing Test Bank
Quiz #1: RN Exams Pharmacology Exams
Quiz #2: RN Exams Medical-Surgical Exams
Quiz #3: RN Exams Fundamentals Exams
Quiz #4: RN Exams Maternal-Newborn Exams
Quiz #5: RN Exams Anatomy and Physiology Exams
Quiz #6: RN Exams Obstetrics and Pediatrics Exams
Quiz #7: RN Exams Fluid and Electrolytes Exams
Quiz #8: RN Exams Community Health Exams
Quiz #9: RN Exams Promoting Health across the lifespan Exams
Quiz #10: RN Exams Multidimensional care Exams
Naxlex Comprehensive Predictor Exams
Quiz #1: Naxlex RN Comprehensive online practice 2019 B with NGN
Quiz #2: Naxlex RN Comprehensive Predictor 2023
Quiz #3: Naxlex RN Comprehensive Predictor 2023 Exit Exam A
Quiz #4: Naxlex HESI Exit LPN Exam
Quiz #5: Naxlex PN Comprehensive Predictor PN 2020
Quiz #6: Naxlex VATI PN Comprehensive Predictor 2020
Quiz #8: Naxlex PN Comprehensive Predictor 2023 - Exam 1
Quiz #10: Naxlex HESI PN Exit exam
Quiz #11: Naxlex HESI PN EXIT Exam 2
Questions on Complications and Interventions
Correct Answer is C
Explanation
<p>Skin traction is not a surgical procedure but rather a non-surgical intervention used in conjunction with other treatments.</p>
Correct Answer is B
Explanation
<p>While skin traction may indirectly support bone healing by reducing pain and allowing proper alignment, it is not the primary goal of this intervention.</p>
Correct Answer is D
Explanation
<p>In skin traction, adhesive straps or wraps are applied to the skin near the fractured area, and weights are attached to create a pulling force. The pulling force helps to align and stabilize the fractured bone.</p>
Correct Answer is B
Explanation
<p>Encouraging active range of motion exercises is not recommended while the patient is in skin traction, as it may disrupt the traction's stabilizing effect on the fractured bone. Passive range of motion exercises may be performed as appropriate, with the healthcare provider's approval.</p>
Correct Answer is D
Explanation
<p>Skin traction is a temporary and short-term intervention used to stabilize a fractured bone and provide pain relief before more definitive treatments, such as casting or surgery, are implemented.</p>
Correct Answer is C
Explanation
<p>Skin traction does not replace the need for surgical interventions for joint dislocations; it is specifically used for fractures.</p>
Correct Answer is C
Explanation
<p>Skin traction is not indicated for muscle strains; it is primarily used for fractures.</p>
Correct Answer is B
Explanation
<p>Skin traction is not contraindicated in patients with chronic orthopedic conditions; however, it may not be the appropriate intervention for their condition.</p>
Correct Answer is A
Explanation
<p>Greenstick fractures are incomplete fractures common in children, and their management may not necessitate skin traction.</p>
Correct Answer is B
Explanation
<p>Skin traction is not used to replace surgical interventions; it is an adjunctive intervention used in conjunction with other treatments for fractures.</p>
Correct Answer is A
Explanation
<p>Dunlop's traction is a type of head and neck traction used for cervical spine injuries. It is not used for hip fractures.</p>
Correct Answer is B
Explanation
<p>Dunlop's traction is a type of head and neck traction used for cervical spine injuries, not lower leg fractures.</p>
Correct Answer is C
Explanation
<p>Dunlop's traction is a type of head and neck traction used for cervical spine injuries, not pediatric femur fractures.</p>
Correct Answer is A
Explanation
<p>Dunlop's traction is a type of head and neck traction, not used for fractures of the lower back or lower extremities.</p>
Correct Answer is B
Explanation
<p>Removing the traction periodically to assess the skin can disrupt the treatment plan and may not be necessary unless there are signs of skin compromise or other complications.</p>
Correct Answer is B
Explanation
<p>Traction cords secured with tape to the bedrails is the appropriate way to secure the traction. This finding does not raise concern.</p>
Correct Answer is C
Explanation
<p>Applying a trochanter roll under the affected hip is not necessary for repositioning with skin traction.</p>
Correct Answer is C
Explanation
<p>Mild tingling sensation in the affected limb can be a common sensation due to traction, and it does not indicate neurovascular compromise.</p>
Correct Answer is D
Explanation
<p>To promote skin integrity, the nurse should instruct the patient to inspect the skin under the traction daily for signs of redness, irritation, or breakdown. Early detection of skin issues can help prevent further complications.</p>
Correct Answer is B
Explanation
<p>Constipation is not directly related to skin traction. It can be caused by various factors, including medications and immobility, but it is not a specific complication of skin traction.</p>
Correct Answer is A
Explanation
<p>Maintaining the traction in a continuous position is a standard practice for skin traction. However, it does not specifically address the prevention of contractures.</p>
Correct Answer is B
Explanation
<p>Faster healing of the injured limb is a desired outcome of effective traction. Inadequate traction may delay healing rather than promote it.</p>
Correct Answer is D
Explanation
<p>An important nursing intervention to prevent complications in a patient with skin traction is to monitor neurovascular status regularly. This includes assessing circulation, sensation, and motion of the affected limb to detect any signs of neurovascular compromise.</p>
Correct Answer is C
Explanation
<p>Excessive traction pressure can occur if the traction is not properly applied or adjusted. However, the primary concern is traction weight displacement, which affects the effectiveness of the treatment.</p>
<p>Requesting physical therapy to assist with range of motion exercises demonstrates effective nursing collaboration. Physical therapists are experts in movement and can provide valuable input in promoting joint mobility for patients in traction.</p>
<p>Providing the healthcare provider with outdated patient data is not effective in patient care and may lead to incorrect decision-making.</p>
<p>Disregarding the physical therapist's recommendations undermines the collaborative effort and diminishes the potential benefits of working together.</p>
<p>Limiting collaboration to only certain team members can create barriers and may result in missed opportunities for valuable input from different perspectives.</p>
<p>Engaging in regular communication to discuss the patient's progress demonstrates effective nursing collaboration. This allows the nurse and physical therapist to coordinate care, make adjustments to the treatment plan, and ensure the best possible outcomes for the patient.</p>
<p>The patient's fractured femur showing signs of healing is not an immediate evaluation parameter for skin traction effectiveness. Skin traction is primarily aimed at reducing pain and realigning the bone.</p>
<p>Deep tissue damage with visible blisters requires immediate intervention. It indicates that the skin is compromised, and the patient is at risk of developing pressure ulcers or skin breakdown. Prompt action is necessary to prevent further damage and ensure patient safety.</p>
<p>Tingling sensation in the toes may be a normal sensation and does not necessarily indicate a complication unless it is accompanied by other neurovascular changes.</p>
<p>The patient stating that the pain is worse with the traction off requires further intervention. Skin traction should relieve pain and discomfort; an increase in pain when the traction is off may indicate inadequate traction or an underlying issue.</p>
<p>The patient having difficulty moving the affected limb may be expected with skin traction, and the nurse should continue to monitor the patient's progress.</p>
<p>Removing the traction periodically to allow the skin to breathe is incorrect. Skin traction is a continuous intervention, and removing it periodically can compromise its effectiveness and may hinder fracture healing.</p>
<p>Option D is the correct instruction because the patient should be vigilant in monitoring for any signs of skin redness, irritation, or discomfort under the traction tape. Promptly reporting these symptoms to the healthcare provider allows for early intervention and prevention of skin complication
No explanation
<p>Option D is essential in maintaining proper traction and alignment. Knots and kinks in the traction ropes can interfere with the traction force, leading to inadequate realignment of the fractured bone.</p>
<p>While skin traction may promote some mobility, its primary purpose is to reduce swelling and discomfort rather than facilitating early ambulation.</p>
<p>Skin traction is typically applied above the fractured area to provide a pulling force in the opposite direction to reduce swelling and discomfort. The traction should not be placed directly over the fractured bone to avoid further injury.</p>
<p>Purplish discoloration below the traction site may indicate impaired circulation, and it requires immediate intervention to prevent further complications like pressure ulcers or nerve damage.</p>
<p>Tingling sensation in the toes may be expected with skin traction, but it does not necessarily indicate a complication unless it is accompanied by other neurovascular changes.</p>
<p>Checking for signs of skin breakdown or pressure sores is essential to prevent complications associated with skin traction. The patient should inspect the skin around the traction site regularly and report any abnormalities to the healthcare provider.</p>
<p>Massaging the skin under the traction tape is not advisable, as it can cause friction and further damage the skin, increasing the risk of skin breakdown.</p>
<p>While skin traction may promote some blood circulation in the affected limb, its primary purpose is to reduce the fracture and stabilize the bone, not to improve circulation.</p>
No explanation
<p>Using the trapeze bar to reposition in bed is an appropriate method for the patient to move independently without compromising the traction's stability.</p>
<p>Visible signs of skin breakdown under the traction tape require immediate intervention. It indicates that the skin is compromised, and the patient is at risk of developing pressure ulcers or skin breakdown. Prompt action is necessary to prevent further damage and ensure patient safety.</p>
Search Here
Related Topics
More on Nursing
Free Nursing Study Materials
Access to all study guides and practice questions for nursing for free.
- Free Nursing Study Trials
- Free Nursing Video tutorials
- Free Nursing Practice Tests
- Free Exam and Study Modes
- Free Nursing Revision Quizlets
