Which action should the nurse implement to reduce the risk of vesicant extravasation in the client who is receiving intravenous chemotherapy?
Instruct the client to drink plenty of fluids during the treatment.
Keep the head of the bed elevated until the treatment is completed.
Monitor the client's intravenous site hourly during the treatment.
Administer an antiemetic before starting the chemotherapy.
The Correct Answer is C
A. Instruct the client to drink plenty of fluids during the treatment.
This option focuses on hydration, which is generally important during chemotherapy to flush out toxins and maintain overall health. However, it does not specifically address the risk of vesicant extravasation.
B. Keep the head of the bed elevated until the treatment is completed.
Keeping the head of the bed elevated is a measure that may be taken for certain conditions or treatments, but it is not directly related to preventing vesicant extravasation.
C. Monitor the client's intravenous site hourly during the treatment.
This is the correct choice. Monitoring the intravenous site for signs of extravasation, such as swelling, redness, or pain, is crucial when administering vesicant chemotherapy drugs. Early detection allows for prompt intervention to minimize potential tissue damage.
D. Administer an antiemetic before starting the chemotherapy.
Administering an antiemetic (a medication to prevent or alleviate nausea and vomiting) is important for managing side effects of chemotherapy, but it does not specifically address the prevention of vesicant extravasation.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
A. Assess client for signs and symptoms of upper airway infection:
While upper airway infections can contribute to respiratory symptoms, the client's history of asthma and the exacerbation of symptoms during exercise suggest that asthma management should be a priority.
B. Determine if the client is using an inhaler before exercising:
This is a relevant consideration, and ensuring proper pre-exercise use of bronchodilators (such as an inhaler) is an important aspect of asthma management. However, the question is broader and involves a review of the client's overall asthma management.
C. Teach client to use pursed lip breathing when episodes occur:
Pursed lip breathing is a technique that can help manage symptoms, especially during episodes of bronchoconstriction. However, the focus here is on a more comprehensive assessment and review of the client's routine asthma management.
D. Review the client's routine asthma management prescriptions:
This is the correct answer. The client's reported symptoms during exercise suggest a potential need for adjustments to the routine asthma management plan. Reviewing the client's prescriptions, including the type and timing of medications, can help ensure optimal control of symptoms, especially during physical activity.
Correct Answer is B
Explanation
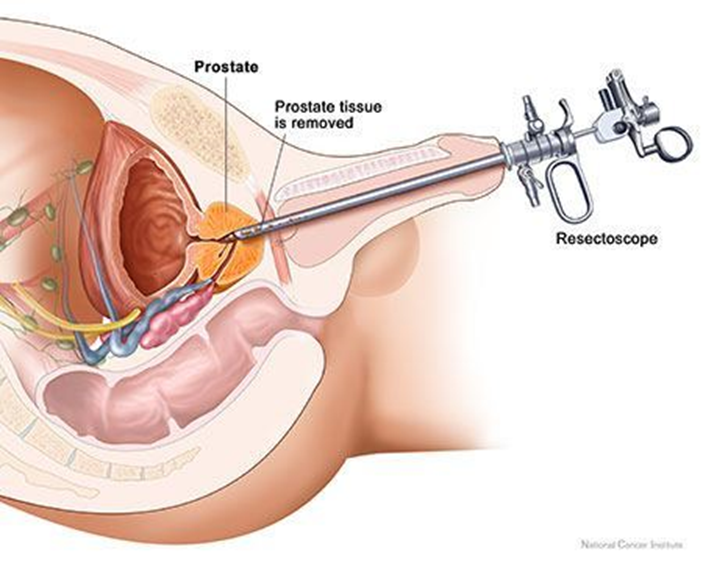
A. Irrigating the catheter manually:
Manually irrigating the catheter without an order may disrupt the clotting process and increase the risk of bleeding. It is not a routine nursing intervention post-TURP without specific orders.
B. Monitoring catheter drainage.
It is not within the nurse's scope of practice to manually irrigate the catheter without a healthcare provider's order, especially in the context of post-TURP care. The dark, pink-tinged outflow with blood clots indicates some expected bleeding following the procedure. The nurse should closely monitor the catheter drainage for the amount, color, and presence of clots.
C. Discontinuing infusing solution:
Discontinuing the normal saline irrigation may lead to clot formation and obstruction, potentially worsening the situation. The continuous bladder irrigation is often used to prevent clot formation and maintain catheter patency post-TURP.
D. Decreasing the flow rate:
The flow rate is typically set by the healthcare provider to maintain catheter patency and prevent clot formation. Decreasing the flow rate without specific orders may not be appropriate in this situation.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
