The unlicensed assistive personnel (UAP) tells the practical nurse (PN) that a resident of the long-term care facility is reporting eye pain and photophobia. The resident is being treated for bacterial conjunctivitis. Upon entering the resident's room, the PN observes that the UAP has darkened the room and placed a warm compress over the resident's eyes. Which action should the PN take?
Turn lights on in the room.
Remove the warm compress.
Elevate the head of the bed.
Offer an oral analgesic.
None
None
The Correct Answer is B
The correct answer is choice B. Remove the warm compress.
Choice A rationale:
Turning the lights on in the room would likely exacerbate the resident’s photophobia (sensitivity to light), causing more discomfort. Photophobia is a common symptom of bacterial conjunctivitis, and keeping the room dim can help alleviate this discomfort.
Choice B rationale:
Removing the warm compress is the correct action. Warm compresses can sometimes be used to relieve symptoms of conjunctivitis, but they are generally more appropriate for viral or allergic conjunctivitis. In the case of bacterial conjunctivitis, warm compresses can potentially worsen the infection by providing a warm, moist environment that promotes bacterial growth. Instead, a cool compress is often recommended to reduce inflammation and discomfort.
Choice C rationale:
Elevating the head of the bed can help reduce swelling and promote drainage, but it is not directly related to the immediate relief of eye pain and photophobia in bacterial conjunctivitis. This action might be more relevant for conditions involving fluid retention or respiratory issues.
Choice D rationale:
Offering an oral analgesic could help manage the resident’s pain, but it does not address the underlying issue of the warm compress potentially worsening the bacterial infection. Pain management is important, but it should be combined with appropriate measures to treat the infection and alleviate symptoms.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Digoxin is a medication used to treat various heart conditions, such as abnormal heart rhythms and heart failure.It works by improving the strength and efficiency of the heart, or by controlling the rate and rhythm of the heartbeat.
One of the important things to monitor when giving digoxin to an infant is the pulse rate. Digoxin can lower the heart rate, which can be dangerous if it becomes too slow.Therefore, the pulse rate should be checked for one full minute before administering digoxin, and the medication should be held if the pulse rate is below 90 beats per minute (bpm) for an infant.
In this case, the infant’s heart rate is 120 bpm, which is within the normal range for a 2-month-old. Therefore, the correct action for the PN to take is to administer the medication and document the heart rate. This is optionbin the list of choices. Optionais incorrect because there is no need to hold the medication or recheck the heart rate in one hour. Optioncis incorrect because there is no need to alert the charge nurse unless there is a problem with the infant’s condition or the medication. Optiondis incorrect because holding the medication and documenting cardiac assessment is not appropriate for a normal heart rate.
Correct Answer is C
Explanation
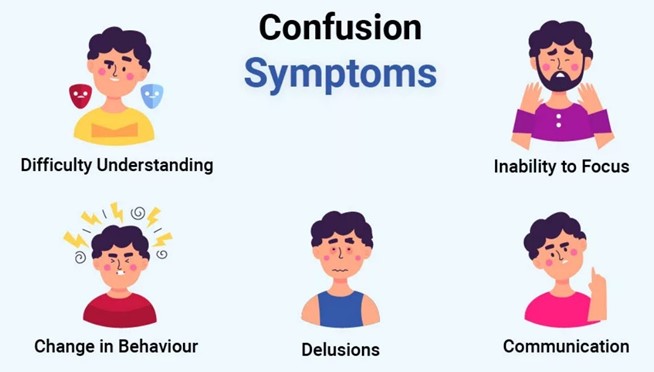
This is the best action for the PN to take because it provides reality orientation and helps the client cope with the change in environment. The client may be experiencing acute confusion or delirium due to stress, medication, infection, or other factors. The PN should remind the client of the date, time, and place frequently and use other strategies such as calendars, clocks, and familiar objects to reduce confusion.
A. Documenting the client's loss of memory in the record is not enough and does not address the client's needs.
B. Notifying the family of the change in the client's condition is not a priority and may not be necessary if the confusion is temporary or reversible.
D. Encouraging the client to rest during the day is not appropriate and may worsen the confusion or disrupt the sleep-wake cycle.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
