The nurse is reviewing the medical electronic record of a client with abdominal aortic aneurysm less than 3 cm in size. Which medical treatment should the nurse anticipate to be prescribed for the client?
Ultrasound every six (6) months.
Intravenous pyelogram yearly.
Assessment of abdominal girth monthly.
Repair of abdominal aortic aneurysm
The Correct Answer is A
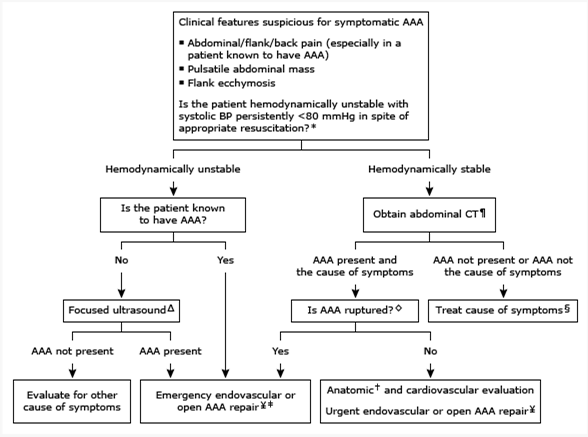
Based on the information provided, the nurse should anticipate that the medical treatment prescribed for a client with an abdominal aortic aneurysm less than 3 cm in size would be regular ultrasound screenings every six (6) months.
Monitoring the size of the abdominal aortic aneurysm through ultrasound is a common approach for managing small aneurysms. Regular ultrasound screenings allow healthcare providers to track the growth rate of the aneurysm and determine if any intervention, such as surgical repair, is necessary as the aneurysm progresses in size.
Let's review the other options and explain why they are not the most appropriate treatments for an abdominal aortic aneurysm less than 3 cm in size:
Intravenous pyelogram yearly: An intravenous pyelogram is an imaging test used to evaluate the urinary system, specifically the kidneys, ureters, and bladder. It is not directly related to the management or monitoring of an abdominal aortic aneurysm.
Assessment of abdominal girth monthly: Assessing the abdominal girth may be a part of the overall assessment of the client's condition, but it is not the primary treatment for managing an abdominal aortic aneurysm. Monitoring the aneurysm size through regular ultrasound screenings is a more specific and accurate approach.
Repair of abdominal aortic aneurysm: Repair of an abdominal aortic aneurysm is typically indicated when the aneurysm reaches a certain size threshold or if it poses a high risk of rupture. For an aneurysm less than 3 cm in size, repair is usually not the initial treatment option. Instead, regular monitoring through ultrasound screenings is recommended to assess the aneurysm's growth rate and determine the appropriate time for intervention.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
The client statement that supports the information of intermittent claudication is: "My legs get a painful cramp when I walk over 30 minutes.": Intermittent claudication is a symptom of peripheral artery disease (PAD) characterized by pain, cramping, or fatigue in the muscles of the lower extremities, typically the calves, thighs, or buttocks. This pain is usually triggered by physical activity, such as walking, and is relieved with rest. The pain is caused by inadequate blood flow and oxygen supply to the muscles due to narrowed or blocked arteries.
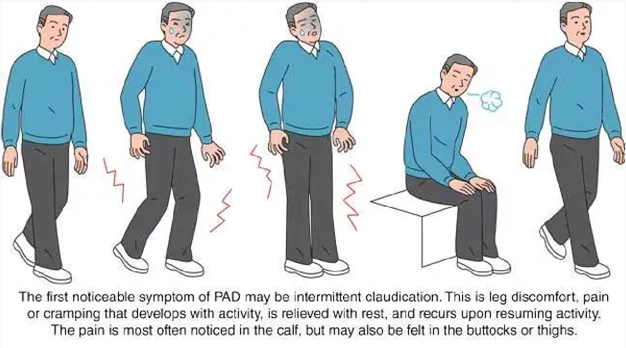
The other client statements do not specifically indicate intermittent claudication:
"My feet feel like I have pins and needles": This sensation of pins and needles is often associated with peripheral neuropathy, which is a condition involving nerve damage and does not directly relate to intermittent claudication.
"When I stand or sit too long, my feet swell": This statement suggests the possibility of venous insufficiency rather than intermittent claudication. Venous insufficiency involves impaired blood return from the legs to the heart and may result in swelling, aching, or heaviness in the legs.
"I get short of breath when I climb a lot of stairs": This symptom is more indicative of cardiovascular or respiratory issues, such as heart or lung disease, rather than intermittent claudication. It suggests that the client may experience exercise intolerance due to cardiopulmonary limitations.
Correct Answer is D
Explanation
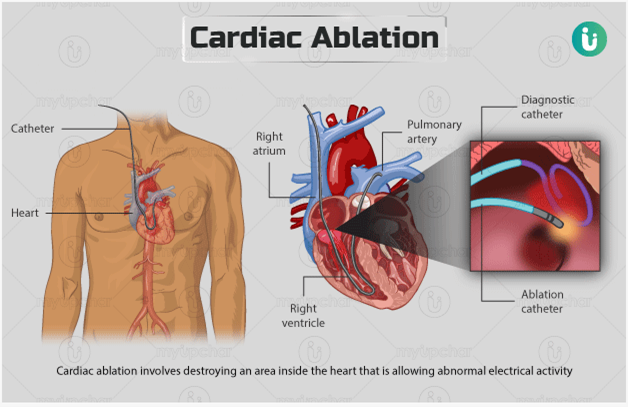
The procedure uses electrical energy to destroy areas of the conduction system: Catheter ablation is a minimally invasive procedure performed to treat abnormal heart rhythms, such as atrial flutter. During the procedure, a catheter is inserted into the heartand used to deliver electrical energy to specific areas of the heart tissue. This energy is used to destroy or ablate the abnormal conduction pathways that are causing the atrial flutter.
Let's go through the other options and explain why they are not accurate:
The procedure stimulates the growth of new pathways between the atria: Catheter ablation does not stimulate the growth of new pathways. Instead, it aims to eliminate or modify existing abnormal pathways in the heart to restore normal electrical conduction.
The procedure uses cold therapy to stop the formation of the flutter waves: Catheter ablation does not use cold therapy. It primarily utilizes radiofrequency energy or other sources of heat to ablate the targeted areas of the heart tissue.
The procedure prevents or minimizes the patient's risk for sudden cardiac death: While catheter ablation can be an effective treatment for certain arrhythmias, including atrial flutter, it is not primarily performed to prevent or minimize the risk of sudden cardiac death. Its main purpose is to restore normal heart rhythm and alleviate symptoms associated with the arrhythmia.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
