The nurse is caring for a client who is taking diclofenac for rheumatoid arthritis. During a clinic visit, the client appears pale and reports increasing fatigue.
Which of the client’s serum laboratory values is most important for the nurse to review?
Total protein.
Hemoglobin.
Glucose.
Sodium.
The Correct Answer is B
Choice A rationale:
Total protein is a measure of the overall protein content in the blood. It includes albumin and globulin.
While it can be helpful in assessing nutritional status and liver function, it is not directly relevant to the client's current symptoms of pallor and fatigue.
Decreased total protein can indicate malnutrition or liver disease, but these conditions would not typically cause the specific symptoms of pallor and fatigue.
Therefore, total protein is not the most important laboratory value to review in this case.
Choice B rationale:
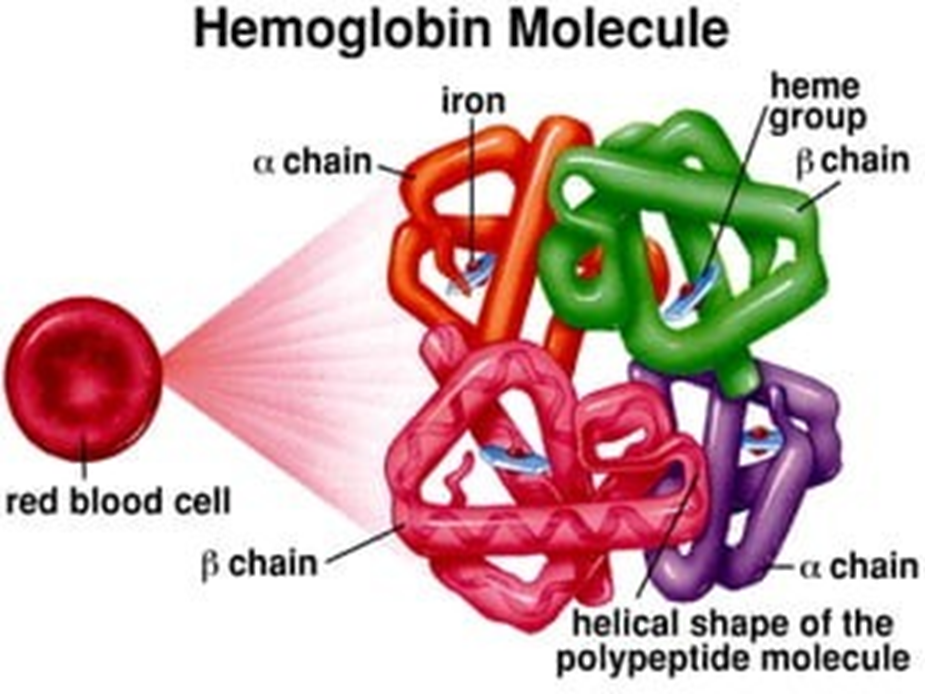
Hemoglobin is the protein in red blood cells that carries oxygen throughout the body.
Paleness (pallor) is a common sign of anemia, which is a condition characterized by a low hemoglobin level. Fatigue is also a common symptom of anemia, as the body's tissues are not receiving enough oxygen.
Diclofenac, a non-steroidal anti-inflammatory drug (NSAID), can cause gastrointestinal bleeding, which can lead to anemia. Therefore, it is essential for the nurse to review the client's hemoglobin level to assess for potential anemia.
Choice C rationale:
Glucose is a type of sugar that the body uses for energy.
Abnormal glucose levels can cause various symptoms, including fatigue. However, glucose levels would not typically cause pallor.
Additionally, there is no indication in the question stem that the client has any risk factors for diabetes or other disorders that affect glucose metabolism.
Therefore, glucose is not the most likely cause of the client's symptoms.
Choice D rationale:
Sodium is an electrolyte that helps regulate fluid balance in the body.
Abnormal sodium levels can cause various symptoms, including fatigue and weakness. However, sodium levels would not typically cause pallor.
Additionally, there is no indication in the question stem that the client has any risk factors for electrolyte imbalances. Therefore, sodium is not the most likely cause of the client's symptoms.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A rationale:
It is true that antibiotics are not effective against viruses like influenza. They only work against bacteria.
However, while providing this information to the client is accurate, it does not directly address the client's inquiry about taking oseltamivir, which is an antiviral medication.
It's essential for the nurse to guide the client toward the appropriate healthcare provider who can assess the client's condition and make an informed decision about whether oseltamivir is a suitable treatment option.
Choice B rationale:
While it is true that influenza vaccination is most effective when given before exposure to the virus, it is still a relevant consideration even after symptoms have begun.
Studies have shown that antiviral medications like oseltamivir can potentially reduce the severity and duration of influenza symptoms, even when started within 48 hours of symptom onset.
Therefore, simply advising the client that it's too late for vaccination without exploring other potential treatment options would be incomplete and potentially disadvantageous to the client's care.
Choice C rationale:
This is the most appropriate response because it ensures that the client receives a comprehensive assessment and individualized treatment plan from a qualified healthcare provider.
The provider can evaluate the client's symptoms, medical history, and potential risk factors to determine if oseltamivir is a suitable medication.
Additionally, the provider can discuss other potential treatment options, such as over-the-counter medications for symptom relief, and provide guidance on self-care measures to promote recovery.
Choice D rationale:
While over-the-counter medications can help manage some symptoms of influenza, such as fever, aches, and cough, they do not directly target the virus itself.
Antiviral medications like oseltamivir can potentially shorten the duration of the illness and reduce the risk of complications, especially in individuals at higher risk.
Therefore, relying solely on over-the-counter medications without considering antiviral therapy could potentially delay recovery and increase the likelihood of adverse outcomes.
Correct Answer is A
Explanation
Choice A rationale:
Liquefying secretions is the most crucial action to address the client's immediate respiratory concerns. Thickened mucus obstructs airflow, leading to shortness of breath, productive cough, and difficulty breathing upon exertion. Increasing fluid intake thins mucus, making it easier to expel and improving ventilation. This directly addresses the client's current symptoms and promotes airway clearance.
Hydration and Mucociliary Clearance: Adequate hydration is indispensable for optimal mucociliary clearance, the natural mechanism that removes mucus from the airways. Fluids moisten the respiratory tract, allowing cilia (tiny hair-like structures) to effectively move mucus upwards, where it can be coughed out or swallowed.
Thinning Mucus: Water acts as a natural expectorant, thinning mucus and reducing its viscosity. This makes it easier for the client to cough up the mucus, clearing the airways and reducing the sensation of breathlessness.
Decreasing Mucus Production: Dehydration can trigger the body to produce more mucus as a protective response. By staying hydrated, the client can help prevent excessive mucus production, further easing symptoms.
Supporting Overall Respiratory Health: Proper hydration maintains the health of the respiratory system's tissues and cells, promoting efficient gas exchange and reducing inflammation.
Preventing Dehydration-Related Complications: Dehydration can exacerbate respiratory problems and lead to other complications, such as fatigue, headaches, and impaired immune function. Maintaining adequate fluid intake helps prevent these issues.
Key points to emphasize to the client:
Drink fluids throughout the day, even if not feeling thirsty.
Water is the best choice, but clear broths, juices, and herbal teas can also contribute to fluid intake. Avoid caffeine and alcohol, as they can be dehydrating.
Monitor urine output to ensure adequate hydration (urine should be pale yellow or clear).
Increase fluid intake during periods of increased mucus production, such as during respiratory infections or exercise.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
