The client was admitted to the medical floor. Upon arrival, the client was assessed: He is difficult to arouse but follows commands. He has a peripheral IV which is infusing normal saline at 145 mL/hr. No redness or edema at the site. Breath sounds are clear and equal bilaterally. He appears pink and well-perfused.
The client had a tonic-clonic seizure that lasted for 3 minutes and 5 seconds. The client became apneic during the seizure and the oxygen saturation dropped to 48%. The client was manually ventilated at 100% oxygen and padding was placed around the vent for safety. After the seizure, the client was turned to his left for recovery.
The physician comes to the bedside following the seizure and prescribes phenytoin. The PN administers the phenytoin as prescribed.
What are the possible toxic effects of phenytoin that the PN should closely monitor the client for after administration?
Select all that apply
Ataxia
Drowsiness
Altered blood coagulation
Anxiety
Aphasia
Vertigo
Visual disturbances
Vomiting
Correct Answer : A,B,C,F,G
Ataxia: Phenytoin can cause problems with coordination and balance, leading to ataxia. The PN should monitor the client for unsteady gait or difficulty with movements.
Drowsiness: Phenytoin can cause drowsiness or sedation. The PN should observe the client for excessive sleepiness or difficulty staying awake.
Altered blood coagulation: Phenytoin can affect blood clotting factors, potentially leading to altered blood coagulation. The PN should assess the client for any signs of bleeding or bruising.
Vertigo: Phenytoin can cause dizziness or vertigo, which is a spinning sensation. The PN should be alert for complaints of dizziness or any difficulty with balance.
Visual disturbances: Phenytoin can cause visual disturbances, such as blurred vision or double vision. The PN should monitor the client's vision and report any changes.
The following options are incorrect regarding the toxic effects of phenytoin:
- Anxiety: Anxiety is not a recognized toxic effect of phenytoin. However, it is important to assess the client for any signs of anxiety or emotional changes.
- Aphasia: Aphasia refers to a language impairment and is not typically associated with the toxic effects of phenytoin.
- Vomiting: While phenytoin can cause gastrointestinal side effects, such as nausea and vomiting, it is not directly related to its toxic effects. However, the PN should still monitor the client for any signs of nausea or vomiting.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
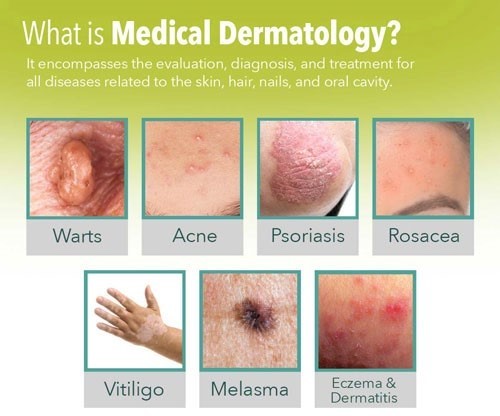
Acne is a common skin condition that often requires specialized treatment. While general skin care practices can help maintain healthy skin, the most appropriate recommendation for a 16-year-old client seeking treatment for acne is to refer them to a dermatologist.
Acne can have various underlying causes, and effective treatment often involves a tailored approach based on the individual's specific condition. Dermatologists are medical professionals specializing in skin health and are best equipped to assess and provide appropriate treatment options for acne.
Correct Answer is A
Explanation
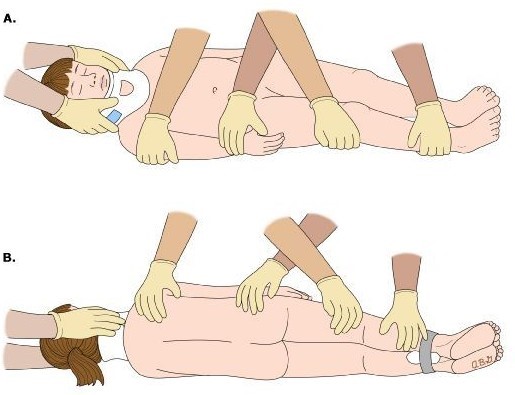
Log-rolling is a technique used to safely turn a client who requires immobilization of the spine or has limited mobility. After log-rolling the client to a lateral position, it is important to maintain proper alignment to prevent injury and promote comfort. Placing pillows strategically can help support and maintain the client's alignment in the lateral position.
The other options mentioned are not the immediate interventions following log-rolling:
B. Raising the head of the bed 30 degrees may be indicated for specific medical conditions or interventions, but it is not the immediate intervention after log-rolling.
C. Flexing the legs and placing a blanket between them is a positioning technique used for preventing skin breakdown and pressure ulcers, but it is not the immediate intervention after log-rolling.
D. Measuring the blood pressure and pulse rate is an important nursing assessment, but it is not the immediate intervention after log-rolling.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
