The client is a 32-year-old multigravida at 28 weeks' gestation, who presents to the obstetrician's office for a routine has given burn three times; once at 35 weeks (twins), once at 38 weeks (singleton) and once at 41 weeks (singleton). All of these children are alive and well. She had one spontaneous abortion at 10 weeks' gestation. Her fourth child weighed 9 pounds (4.08 kg) at 41 weeks gestation.
The client is at 28 weeks. She has been receiving prenatal care since 8 weeks gestation. Her fasting 1-hour glucose screening level, which was done 1 week prior, is 164 mg/dL (9.1 mmol/L). Her 3-hour oral glucose tolerance test results reveal a fasting blood sugar of 168 mg/dL (9.3 mmol and a two-hour postprandial of 220 mg/dL (12...mol/L).
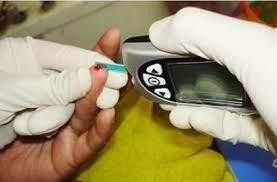
Scheduled the client to meet with the obstetrician, Diabetic Nurse Educator, and a Registered Dietician for the next day. After a discussion about gestational diabetes and seeking the client's input, a suggested plan of care is outlined, which includes dietary control and glucose self-monitoring.
The registered dietician (RD) discusses the need to
Choose the most likely options for the information missing from the statement(s) by selecting from the lists of options provided.
The diabetic nurse educator instructs the client to perform fingerstick blood glucose (FSBG) monitoring Select Response
of the night at bedtime and in the middle
prior to each meal
every two hours throughout the day
during the middle of the night
The Correct Answer is B
A) Incorrect- While bedtime monitoring is important, the frequency described in this choice is not consistent with FSBG monitoring before meals.
B) Correct- Performing FSBG monitoring before each meal helps the client track her blood glucose levels before consuming food, allowing her to adjust her diet or insulin regimen if necessary.
C) Incorrect- Monitoring every two hours may be excessive and not necessary for managing gestational diabetes.
D) Incorrect- Monitoring during the night is important for glycemic control, but it doesn't specifically address the need to monitor before meals.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
A. Explaining the procedure and obtaining the signature is the provider’s responsibility, not the practical nurse’s.
B. Checking the medical record for a signed consent form is part of the practical nurse’s verification role but does not address assessing client understanding.
C. Obtaining consent from a family member is only appropriate if the client is unable to provide it; otherwise, consent must come directly from the client.
D. The practical nurse is responsible for ensuring the client understands the procedure and the purpose of the consent form, reinforcing the provider’s explanation and promoting informed consent.
Correct Answer is ["B","C","D"]
Explanation
Client's pain rating on a scale of 1 to 10: This information helps assess the client's current pain level and determine the need for pain medication.
Time of the last administration of pain medication: This is important to avoid overdosing or administering pain medication too frequently. It helps ensure that pain medication is given at the appropriate time intervals.
Effectiveness of the last pain medication administered: Understanding whether the previous dose provided relief or not helps guide the choice of the next medication or dosage.
The other options are not directly related to the immediate decision of administering pain medication:
Height and weight of the client prior to admission may be part of the client's medical history but are not typically required information just before administering pain medication.
A history of pain medication use during the past year is important information but may be already documented in the client's medical records and not necessary to obtain immediately before administration.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
