A nurse is assessing a client who has peripheral venous disease. Which of the following findings should the nurse recognize as a manifestation of venous disease?
Swollen and enlarged veins.
Loss of pigmentation over the shin area.
Shiny appearance to the lower extremities.
Diminished hair growth on the lower extremities.
The Correct Answer is A
Choice A Reason:
Swollen and enlarged veins, also known as varicose veins, are a common manifestation of peripheral venous disease (PVD). This condition occurs when the valves in the veins become weak or damaged, leading to blood pooling and increased pressure within the veins. This results in the veins becoming enlarged, twisted, and visible under the skin1. Varicose veins can cause discomfort, pain, and a heavy feeling in the legs. They are often exacerbated by prolonged standing or sitting and can be a cosmetic concern as well.
Choice B Reason:
Loss of pigmentation over the shin area is not typically associated with peripheral venous disease. This symptom is more commonly seen in conditions such as chronic venous insufficiency (CVI), where prolonged venous hypertension leads to skin changes, including hyperpigmentation and lipodermatosclerosis. However, it is not a primary manifestation of PVD itself.
Choice C Reason:
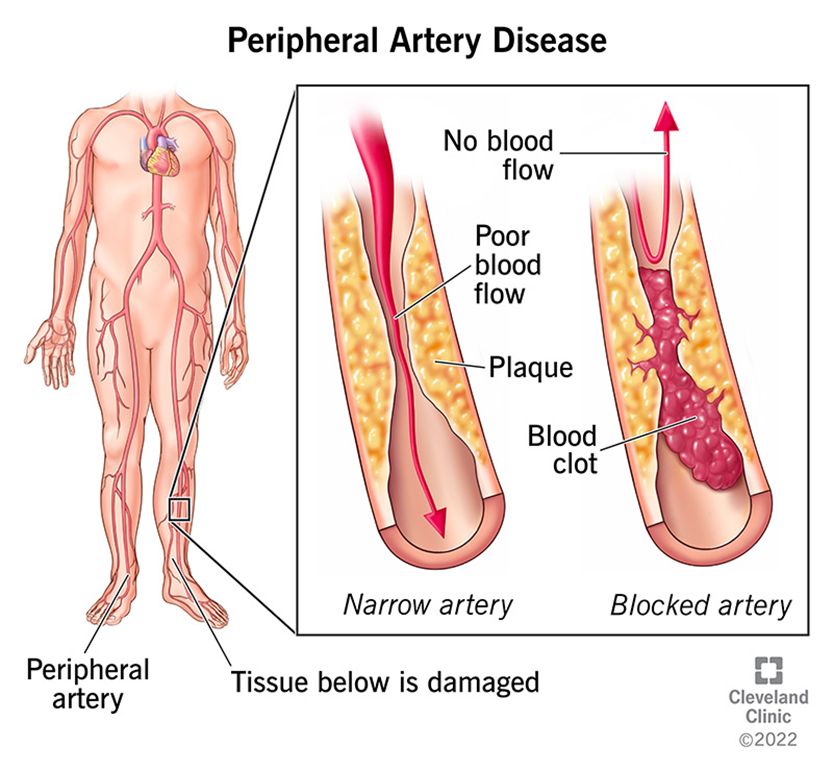
A shiny appearance to the lower extremities is more commonly associated with peripheral arterial disease (PAD) rather than peripheral venous disease. In PAD, reduced blood flow to the extremities can cause the skin to become thin, shiny, and hairless. This is due to the lack of oxygen and nutrients reaching the skin and underlying tissues. In contrast, PVD primarily affects the veins and does not typically cause these skin changes.
Choice D Reason:
Diminished hair growth on the lower extremities is another symptom more commonly associated with peripheral arterial disease (PAD). In PAD, the reduced blood flow to the extremities can lead to hair loss, as the hair follicles do not receive adequate oxygen and nutrients. Peripheral venous disease, on the other hand, does not usually cause hair loss. Instead, it is characterized by symptoms related to venous insufficiency, such as varicose veins, swelling, and skin changes.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["D"]
Explanation
Choice A Reason:
A urine specific gravity of 1.010 falls within the normal range of 1.005 to 1.0301. This value does not indicate hyponatremia. In SIADH, urine is often more concentrated due to the retention of water, leading to higher specific gravity values.
Choice B Reason:
Respiratory alkalosis is not a typical manifestation of hyponatremia. It is usually associated with conditions that cause hyperventilation, such as anxiety or high altitude. SIADH typically does not cause respiratory alkalosis.
Choice C Reason:
Diarrhea is not a direct manifestation of hyponatremia. While diarrhea can lead to electrolyte imbalances, including hyponatremia, it is not a symptom caused by SIADH5. SIADH leads to water retention and dilutional hyponatremia, not diarrhea.
Choice D Reason:
Diminished reflexes are a manifestation of hyponatremia. Low sodium levels affect neuromuscular function, leading to symptoms such as muscle weakness, cramps, and diminished reflexes7. This is a direct result of the electrolyte imbalance caused by SIADH.
Correct Answer is C
Explanation
Choice A Reason:
While monitoring the frequency of urination is important for managing diabetes insipidus, it is not the most critical aspect of discharge teaching. Diabetes insipidus causes excessive urination, and patients should be aware of this symptom. However, understanding the importance of wearing a medical alert bracelet is more crucial for ensuring immediate and appropriate care in emergencies.
Choice B Reason:
Changes in appetite are not a primary concern for patients with diabetes insipidus. The condition primarily affects fluid balance and urine output rather than appetite. Therefore, this topic is less relevant compared to the need for a medical alert bracelet.
Choice C Reason:
The benefit of a medical alert bracelet is paramount for patients with diabetes insipidus. In case of an emergency, the bracelet can inform healthcare providers about the patient’s condition, ensuring they receive appropriate and timely treatment. This can be life-saving, especially if the patient is unable to communicate their medical history.
Choice D Reason:
Weight gain or loss can be a secondary concern for patients with diabetes insipidus, as the condition primarily affects fluid balance. While it is important to monitor weight to assess fluid status, it is not as critical as ensuring the patient understands the importance of wearing a medical alert bracelet.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
